update December 19 2023 by Eddie Tannenbaum BA (Univ of Iowa School of Medicine) and Shaun Edalati BS (Mount Sinai School of Medicine)
return to: Common Call Problems
see also: Tonsillectomy and Adenoidectomy
Background
Peritonsillar abscess continues to be the most common deep head and neck infection (Galioto 2008). Pus can build up between the pharyngeal muscles and the palatine tonsil capsule, resulting in peritonsillar abscesses (Long & Gottlieb 2023). The tonsil's upper portion is most affected, then its middle and lower portions. It may be brought on by a Weber gland blockage or a history of tonsillitis or throat infection (Galioto 2008). Peritonsillar abscesses are often polymicrobial, including anaerobic bacteria like Fusobacterium necrophorum and streptococcal and staphylococcal species (Klug 2014). The frequency of peritonsillar abscess is highest in those aged 15-19, reaching 167 per 100,000. It occurs yearly in approximately 30 out of every 100,000 individuals aged 5 to 49 (Klug 2014).
If left untreated, infections can lead to severe complications and even death. Conditions such as descending mediastinitis, parapharyngeal and retropharyngeal abscesses, necrotizing fasciitis, internal jugular vein suppurative thrombophlebitis, and airway blockage may result in serious consequences if not properly addressed (Klug 2020). Mortality rates from these serious complications could reach 10% (Klug 2020). Early diagnosis and treatment are therefore is important (Long & Gottlieb 2023).
Evaluation
- History:
- Sore throat
- Decreased oral intake due to progressive odynophagia
- Drooling from inability to tolerate own secretions
- Fever
- Voice changes- "hot potato voice"
- Neck swelling and pain (Galioto 2008)
- Ipsilateral otalgia
- Malaise
- PMH – specific concerns to addres include: diabetes, medication allergies, recent trial of antibiotics, frequency and severity of recurrent infectious pharyngitis, snoring or other symptoms of obstructive sleep apnea (Wald 2023).
- Physical exam
- Airway assessment
- Trismus (sine qua non of PTA) - due to inflammation causing medial pterygoid spasm.
- Asymmetry of soft palate with uvular deviation
- Neck ROM
- Quality of voice
- Lymphadenopathy
- Workup:
- Labs: Not required but may help assess severity and guide management, CBC, serum electrolytes. If drainage is performed, gram stain, culture, and susceptibility testing of abscess fluid may assist with antimicrobial therapy for immunocompromised patients (Wald 2023).
- Imaging
- Not always required but commonly performed - consider CT scan if significant decreased neck ROM with pain on turning, to assess posterior pharyngeal space involvement, or if findings are unusual (eg. bilateral swelling)
- CT: Look for a rim-enhancing fluid collection in the peritonsillar space
- “Peritonsillar abscess,” by James Heilman, MD, free access - licensed under CC BY-SA 4.0, via Wikimedia Commons
-
Ultrasonography (US) may be helpful in distinguishing peritonsillar abscess from peritonsillar cellulitis (Kim et al. 2023). Look for an echo-free cavity with an irregular border whereas peritonsillar cellulitis appears homogeneous or striated with no clear fluid collection (Wald 2023).
Improved outcomes have been reported to be associated with use of US prior to needle aspiration (Costantino et al. 2012).
Cultures may not be required and may commonly show oral flora. If drainage is performed, gram stain, culture, and susceptibility testing of abscess fluid may assist with antimicrobial therapy for immunocompromised patients (Wald 2023).
Consider rapid Strep antigen testing
Management
- Initial management
- Antibiotics
- Consensus guidelines have not been established for the management of PTA and there is variability in the choice of antibiotic therapy (Wu et al. 2021). PTAs have been found to commonly contain a mixture of Gram-negative and Gram-positive bacteria, including both anaerobes and aerobes (Moen et al. 2023). The most frequently identified aerobes are Group A streptococcus and Streptococcus milleri group while the most common isolated anaerobe is Fusobacterium necrophorum (Galioto 2017). Other typical bacteria include Corynebacterium, Staphylococcus aureus, Bacteroides, Peptostreptococcus, and Prevotella (Galioto 2017).
- Penicillin alone has been found to be effective for the routine care of otherwise healthy adult patients in combination with drainage and supportive care (Herzon, 2018). However, broad-spectrum antibiotics are often utilized as first-line therapy given the polymicrobial composition and rates of penicillin-resistant organisms of PTAs (Galioto 2017). Some of the most commonly prescribed antibiotics for the management of PTA include amoxicillin‐clavulanic acid and clindamycin (Wu et al. 2021). A comparative summary from a compilation of the following references is included in the table below: Galioto, 2017; Wald, 2023; Micromedex 2023.
- Antibiotics
- IV fluid rehydration (eg. Lactated Ringers)
- Steroids
- The use of steroids in the management of PTA continues to be debated but some evidence seems to support that adjunctive, high-dose, short-term use is safe and beneficial (Kent et al., 2019).
- May consider hold due to mitigating circumstances such as diabetes given effect on glucose
- A compilation from references: Chau et al., 2014; Kent et al., 2019; Koçak.et al., 2017; Mirvakili et al., 2009; Ozbek et al., 2004; and Shaikh, 2008. The values noted below include all consistent recommendations or synthesized ranges, with the exception of methylprednisolone dose of 1 mg/kg from Koçak.et al. and only Ozbek et al. reported maximum methylprednisolone dose, which was 250 mg total.
|
Steroid |
Route of administration |
Dose |
|
Methylprednisolone |
Intravenous |
2-3 mg/kg |
|
Dexamethasone |
Intravenous |
8-10 mg |
- Pain medication (eg. morphine/Dilaudid)
- Optimum management of PTA is controversial. Options include:
- Needle aspiration only
- Incision and drainage
- Quincy tonsillectomy
- Disposition: Often discharge home after drainage/tonsillectomy if patient can drink, is breathing well, not septic, and is not actively bleeding
- Home Rx:
- Give elixir form if possible
- Oral antibiotic per above for 10-14 days
- Pain (eg. Lortab 5/500 1-2 tab po q4h)
- Saltwater rinses, soft diet for a few days
- Consider 2-3 days of 20-30mg prednisone
|
Study |
Therapy Recommendations |
|
Galioto 2017 |
IV
Oral
Continue therapy for 10-14 days |
|
Wald 2023 |
IV
Oral
|
|
Micromedex 2023 |
Mild disease
Moderate to severe disease
|
Drainage procedure
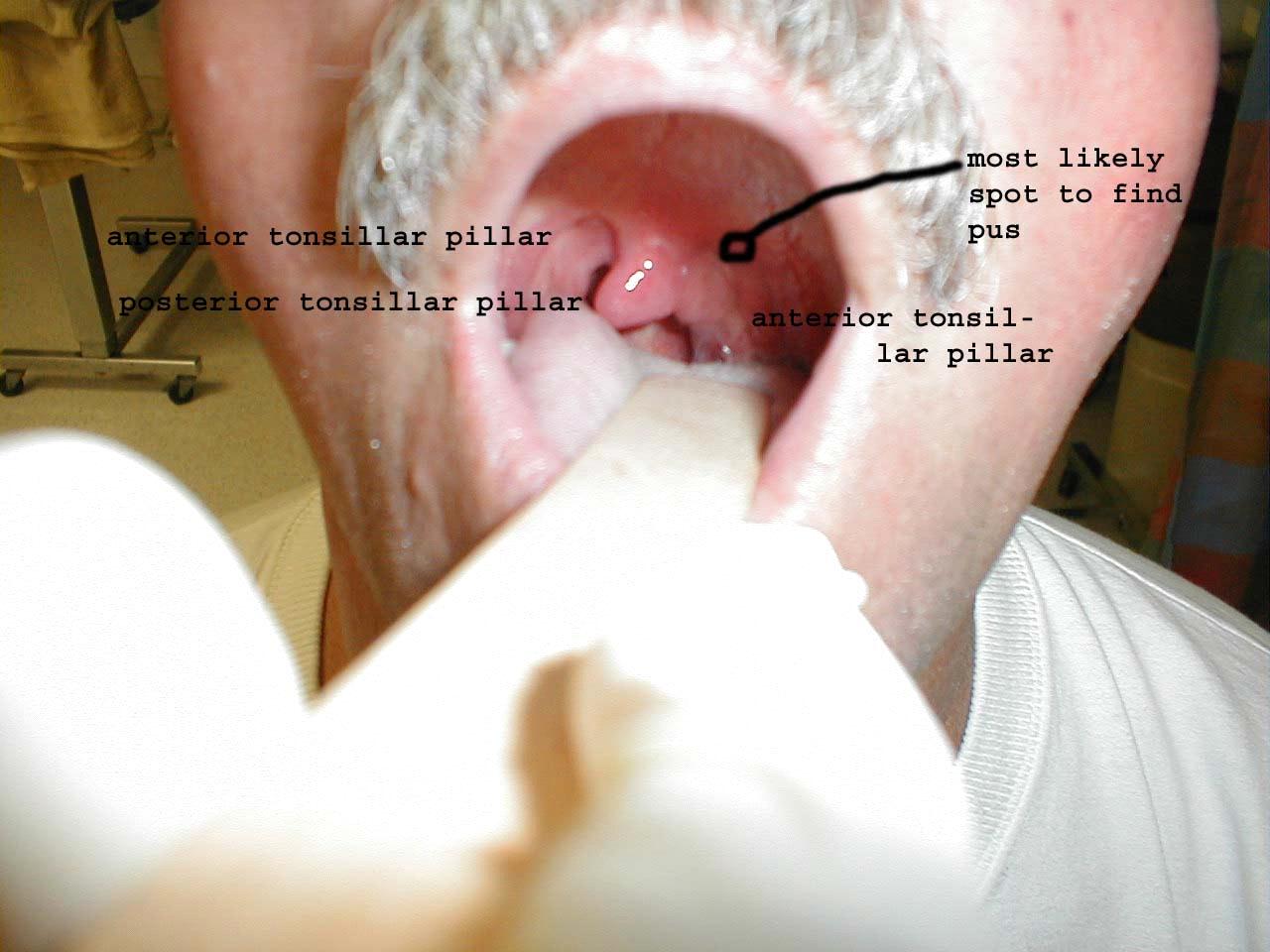
- Anatomic considerations
- Target: abscess is usually superior to the tonsil, at the intersection of the base of the uvula and the anterior tonsillar pillar (see circled area in diagram below), and deep to the mucosa and palatoglossus muscle.
- The carotid is usually 2.0-2.5cm posterolateral to the target.
- May consider bending the needle at 1.5cm or cutting off the a needle cap to expose only 1.5cm of needle
- Equipment
- Hurricaine spray and/or 4% viscous lidocaine, 1% lidocaine with 1:100,000 epinephrine
- 3cc syringe with 18g needle (for drawing lidocaine) and 27g needle (for injection)
- Control top syringe with 18g needle
- #11 blade
- Hemostat
- Suction with Yankauer tip
- Headlamp
- Informed consent
- Patient positioning – operator preference
- Sitting
- Lying (ref 1)
- Local anesthesia
- Topical (eg. hurricaine spray, viscous lidocaine)
- Consider IV morphine, versed
- Inject 1% lidocaine with 1:100,000 to mucosa, then deeper into muscle
- Have Yankauer suction ready in case pus drains with injection to decrease risk of patient aspirating the pus
- Needle drainage
- If pus drained with the lidocaine injection, aim for that area, otherwise aim for the target as described above.
- Insert needle on control top syringe about 1cm, constantly pulling back while advancing.
- Aspirate as much as possible. It may be necessary to redirect the needle to different angles, or try other spots.
- Remember to avoid directing the needle laterally and more than 2cm deep to decrease risk of encroaching on the carotid artery
- Incision and drainage
- If an abscess pocket is identified, withdraw the needle and make an incision about 1cm long following the orientation of the arch.
- Spread in the pocket using hemostats and break up any septations.
- The Yankauer tip can be used to apply gentle pressure around the incision site to facilitate further drainage.
- The incision should be left open as possible to allow for continued drainage
- Consider obtaining bacterial culture (Most common single organism implicated is S. pyogenes, however, cultures demonstrating mixed oral flora are quite common)
References
Chang and Hamilton. Novel technique for peritonsillar abscess drainage. Ann Otol Rhinol Laryngol (2008) vol. 117 (9) pp. 637-40
Chau JK, Seikaly HR, Harris JR, Villa-Roel C, Brick C, Rowe BH. Corticosteroids in peritonsillar abscess treatment: a blinded placebo-controlled clinical trial. Laryngoscope. 2014;124(1):97-103. doi:10.1002/lary.24283
Costantino TG, Satz WA, Dehnkamp W, Goett H. Randomized trial comparing intraoral ultrasound to landmark-based needle aspiration in patients with suspected peritonsillar abscess. Acad Emerg Med. 2012;19(6):626-631. doi:10.1111/j.1553-2712.2012.01380.
Galioto NJ. Peritonsillar abscess. Am Fam Physician. 2008;77(2):199-202.
Galioto NJ. Peritonsillar Abscess. Am Fam Physician. 2017;95(8):501-506.
Heilman J. File:PeritonsilarAbsMark.png. Wikimedia Commons. October 29, 2020. Accessed November 17, 2023. https://commons.wikimedia.org/wiki/File:PeritonsilarAbsMark.png.
Herzon FS, Meiklejohn DA, Hobbs EA. What antibiotic should be used in the management of an otherwise healthy adult with a peritonsillar abscess?. Laryngoscope. 2018;128(4):783-784. doi:10.1002/lary.26881
Kent S, Hennedige A, McDonald C, et al. Systematic review of the role of corticosteroids in cervicofacial infections. Br J Oral Maxillofac Surg. 2019;57(3):196-206. doi:10.1016/j.bjoms.2019.01.010
Kim DJ, Burton JE, Hammad A, et al. Test characteristics of ultrasound for the diagnosis of peritonsillar abscess: A systematic review and meta-analysis. Acad Emerg Med. 2023;30(8):859-869. doi:10.1111/acem.14660
Klug TE. Incidence and microbiology of peritonsillar abscess: the influence of season, age, and gender. Eur J Clin Microbiol Infect Dis. 2014;33(7):1163-1167. doi:10.1007/s10096-014-2052-8
Klug TE, Greve T, Hentze M. Complications of peritonsillar abscess. Ann Clin Microbiol Antimicrob. 2020;19(1):32. doi:10.1186/s12941-020-00375-x
Koçak HE, Acıpayam H, Elbistanlı MS, et al. Is corticosteroid a treatment choice for the management of peritonsillar abscess?. Auris Nasus Larynx. 2018;45(2):291-294. doi:10.1016/j.anl.2017.04.008
Long B, Gottlieb M. Managing Peritonsillar Abscess. Annals of Emergency Medicine.2023;82(1):101-107. doi:10.1016/j.annemergmed.2022.10.023
Micromedex. Peritonsillar abscess. Accessed November 26, 2023. https://www-micromedexsolutions-com.proxy.lib.uiowa.edu/micromedex2/libr...
Mirvakili A, Owlia M, Atighechi S, et al. Effect of corticosteroids in routine treatment of peritonsillar abscess. J Shahid Sadoughi Univ Med Sci 2009;16:10–5.
Moen CM, Paramjothy K, Williamson A, et al. A systematic review of the role of Penicillin versus penicillin plus metronidazole in the management of peritonsillar abscess. The Journal of Laryngology & Otology. 2023;137(9):992-996. doi:10.1017/s0022215123000804
Ozbek C, Aygenc E, Tuna EU, Selcuk A, Ozdem C. Use of steroids in the treatment of peritonsillar abscess. The Journal of Laryngology & Otology. 2004;118(6):439-442. doi:10.1258/002221504323219563
Shaikh KR. Treatment of peritonsillar abscess and role of steroids. Journal of Liaquat University of Medical & Health Sciences. 2008;7(1):31-33. doi:10.22442/jlumhs.08710139
Steyer TE. Peritonsillar abscess: diagnosis and treatment [published correction appears in Am Fam Physician 2002 Jul 1;66(1):30]. Am Fam Physician. 2002;65(1):93-96.
Wald ER. Peritonsillar cellulitis and abscess. UpToDate. October 8, 2023. Accessed November 11, 2023. https://www.uptodate.com/contents/peritonsillar-cellulitis-and-abscess?s....
Wu V, Manojlovic Kolarski M, Kandel CE, Monteiro E, Chan Y. Current trend of antibiotic prescription and management for peritonsillar abscess: A cross-sectional study. Laryngoscope Investig Otolaryngol. 2021;6(2):183-187. Published 2021 Mar 11. doi:10.1002/lio2.538
Other Online Resources:
Sanford Guide. Peritonsillar abscess. Antimicrobial Therapy, Inc. (version 6.4.9) [Mobile app]. App store. https://apps.apple.com/us/app/sanford-guide/id863196620
Epocrates. Peritonsillar/tonsillar abscess. Athenahealth (version 23.11.0) [Mobile app]. App store. https://apps.apple.com/us/app/epocrates/id281935788