Return to: Hypoglossal Nerve Stimulator Implantation (Selective Upper Airway Stimulation); Obstructive Sleep Apnea (OSA)
John Henrich BS with assistance from Douglas Van Daele MD
Initially compiled 9-27-2021 by Henrich and Van Daele with future adaptations per additional contributors
General Considerations
- Obstructive sleep apnea (OSA) is a common breathing disorder with an estimated 17% of women and 34% of men, ages 30-70, having at least mild disease in the US (Gottleib 2020).
- The prevalence of OSA has increased by 30% over the last 20 years and is expected to continue to increase in the future due to its association with the obesity epidemic.
- OSA may be associated with comorbidities including hypertension, diabetes, atrial fibrillation, heart failure, CAD, stroke, and death. It is also associated with reduced quality of life, impaired work performance, and increased risk of motor vehicle accidents.
- Many consider the gold standard in OSA management to be CPAP therapy. However CPAP intolerance is common - with one study (Russel 2015) (n=616), demonstrating that 44% of patients were not adherent to therapy after 3 years. Other studies estimate this rate to be between 29-83% (Gottleib 2020).
- Traditionally surgery to address OSA has employed techniques to remove redundant tissue (tonsils/palate/base of tongue) or to tighten floppy tissue in the upper airway. Hypoglossal nerve stimulation (HNS) is a newer surgical approach that works instead by enhancing neuromuscular tone in the upper airway.
- Nighttime loss of neuromuscular tone is proposed to be a primary pathophysiological basis for OSA (Gottleib 2020).
- Hypoglossal nerve stimulation has been shown to produce significant objective and subjective improvements in OSA symptoms for select patient populations.
- The STAR trial (STAR = Stimulation therapy for apnea reduction; n=126; multicenter prospective RCT, following patients receiving Inspire HNS device) demonstrated a 78.8% reduction in AHI, 65.7% reduction of the oxygen desaturation index, and a 40.5% reduction of the Epworth Sleepiness Scale (ESS; subjective measure) after 5 years (Woodson 2018).
- A meta-analysis of 12 studies demonstrated a mean reduction of -17.4 for AHI, -14.7 for ODI, and -5.36 for ESS in patients with HNS therapy (Constantino 2020).
- The Hypoglossal Nerve Stimulator (HNS) has been reported to have a good safety profile.
- Data from the ADHERE registry (ongoing international multicenter prospective observational study, following patients receiving Inspire HNS device) demonstrated that the combined rate of severe adverse events (i.e., infection, speech problems, tongue weakness, revision interventions, neuropraxia, and pneumothorax) was approximately 1% (Heiser 2019). The most common side effect was discomfort associated with electrical stimulation.
- A recent meta-analysis (Neruntarat 2021) reported HNS to be more effective than traditional OSA surgeries in managing OSA for selected patients.
- This meta-analysis comparing HNS to traditional OSA surgeries demonstrated that patients who received HNS had a significantly greater AHI reduction (23.9 vs 15.8; P < 0.001) as well as a significantly greater reduction of the oxygen desaturation index when compared to the traditional surgery group (Neruntarat 2021).
- HNS patients also had significantly shorter hospital stays, lower readmission rates, and less overall adverse events than the traditional surgical group (Neruntarat 2021).
- Another study which compared traditional pharyngeal OSA surgery (data obtained from the National Surgery Quality Improvement Program) to HNS (data obtained from ADHERE registry) demonstrated that HNS recipients had lower postoperative complication rates compared to their traditional OSA surgery counterparts (Van Daele 2021).
- HNS recipients had significantly shorter hospital stays, lower thirty-day return to operating room rates (0.1% HNS vs 4.8% traditional surgical group), and less surgical site infections (0.13% HNS vs 0.9% traditional surgical group) (Van Daele 2021).
- Currently (9-27-2021) the only FDA cleared HNS device is the unilateral hypoglossal stimulator made by Inspire. This Inspire device is the focus of discussion.
- Other HNS devices include the ImThera HNS, Nyxoah Genio HNS and Transcutaneous Nerve Stimulators.
- ImThera device stimulates both the tongue protrusors and retractors (unlike Inspire) and is currently in a clinical trial set to be completed in 2022.
- The ImThera device is constantly on during the night, unlike the Inspire device which is timed with respiration.
- Nyxoah Genio device produces bilateral stimulation and is unique in that it requires only one incision and is controlled by an external unit that activates a small implanted battery free submental stimulator.
- The Genio device is currently begin evaluated by an ongoing trial in an attempt to get FDA approval, with enrollment target to be completed in early 2022.
- A small open label study with the Genio device demonstrated a significant reduction in the AHI of 46%, a 49% reduction of the oxygen desaturation index, and a 27% reduction of the ESS (Eastwood 2020).
- Transcutaneous nerve stimulators work by placing a non-invasive patch on the submental area, thereby indirectly stimulating genioglossus at night to open the airway.
- A meta-analysis with transcutaneous stimulators demonstrated a mean reduction in AHI of -16.5 (46% overall reduction), however no significant change in the oxygen desaturation index or the ESS was observed (Ratneswaran 2020).
- This study also concluded that invasive HNS therapy was more effective with a mean reduction in AHI of -24.9 (66% overall reduction), as well as a significant reduction in the oxygen desaturation index and ESS.
- A meta-analysis with transcutaneous stimulators demonstrated a mean reduction in AHI of -16.5 (46% overall reduction), however no significant change in the oxygen desaturation index or the ESS was observed (Ratneswaran 2020).
- ImThera device stimulates both the tongue protrusors and retractors (unlike Inspire) and is currently in a clinical trial set to be completed in 2022.
- A recent study has demonstrated that sternothyroid muscle contraction via ansa cervicalis stimulation was able to significantly increase retropalatal cross sectional area (CSA) in patients with OSA (211% increase in CSA, p < 0.05) (Kent 2021).
- Furthermore, this same study demonstrated that supplementing HNS with ansa cervicalis stimulation produced a significantly greater increase in retropalatal CSA than isolated HNS therapy (180% increase in CSA with HNS + ACS therapy versus isolated HNS therapy, p < 0.05).
- These results suggest that ansa cervicalis stimulation may augment HNS efficacy by decreasing pharyngeal collapsibility.
- Other HNS devices include the ImThera HNS, Nyxoah Genio HNS and Transcutaneous Nerve Stimulators.
Inspire Hypoglossal Nerve Stimulator Components
- Has 3 components that are placed in 2 incisions (previously 3 incisions were used).
- Stimulating lead
- This lead is placed around the medial branches of the hypoglossal nerve (discussed below) and initiates contraction of the tongue muscles thus opening the upper airway.
- Sensing lead
- This lead is placed between the internal and external intercostals to detect respiratory effort.
- It then sends a signal to the generator.
- Pulse Generator
- Receives input from the sensing lead during respiration initiation and sends an impulse to stimulating lead opening the upper airway.
- Stimulating lead
Anatomy
- In addition to the standard surgical background to address Level IA and B, more extensive knowledge of branching patterns of the hypoglossal nerve and innervation of tongue musculature is needed to perform this procedure.
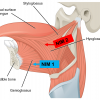
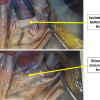
- The Inspire stimulating cuff is to be placed around the branches of the hypoglossal nerve that innervate muscles of tongue protrusion, while excluding branches that retract the tongue (see Figure 2).
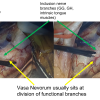
- The vasa nevorum usually sits at the division of these functional branches and serves as a useful landmark (see Figure 2).
- Inclusion branches:
- Genioglossus (GG)
- Transverse and vertical intrinsic tongue muscles (T/V)
- Geniohyoid (GH)
- Exclusion branches:
- hyoglossus (HG)
- styloglossus (SG)
- Additional neck anatomy (see Figure 3)
- HGN Exposure:
- To gain exposure of the hypoglossal nerve, first the anterior-inferior border of the submandibular gland must be dissected free. Then the digastric tendon and the posterior border of mylohyoid are retracted, exposing the nerve.
- Adjacent nerves and position relative to HGN at incision:
- Lingual nerve (superior and deep)
- Marginal mandibular nerve (superficial)
- HGN Exposure:
- The Inspire stimulating cuff is to be placed around the branches of the hypoglossal nerve that innervate muscles of tongue protrusion, while excluding branches that retract the tongue (see Figure 2).
- Chest incision anatomy
- Dissection is done through the pectoralis major and if needed the serratus anterior muscle to expose the external intercostal muscle (fibers run superior-laterally to inferior-medially) and internal intercostal muscle (fibers run inferior-laterally to superior-medially).
Preoperative Preparations
- Evaluation
- Physical assessment of surgical sites (neck and chest) with detailed head and neck exam.
- Assessment of existing implantable devices (pacemaker, ICD, spinal cord stimulator, vagus nerve stimulator, etc.)
- A study of 14 patients with an existing pacemaker or ICD who underwent HNS surgery did not reveal any device-device interactions after 1 year (Parikh 2018).
- If another device is implanted the HNS should be placed on the opposite side (Inspire company recommends at least 15 cm apart).
- Future studies need to assess for interactions with other devices.
- A study of 14 patients with an existing pacemaker or ICD who underwent HNS surgery did not reveal any device-device interactions after 1 year (Parikh 2018).
- Social history: Inspire recommends consideration for implanting HNS on the right side (standard convention is the left) if the patient shoots weapons and places the butt of the weapon close to the generator.
- Current (9-07-2021) inclusion criteria:
- 18 years of age and older
- Diagnosed with moderate-to-severe OSA (AHI 15-65)
- As determined by home or laboratory polysomnogram
- CPAP failure or inability to tolerate CPAP
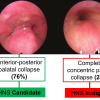
- Appropriate airway anatomy, as assessed by drug induced sleep endoscopy (DISE).
- Complete concentric palatal collapse (see Figure 4) occurs in up to 24% of patients evaluated by DISE and is ineligible for HNS as studies have demonstrated a very low success rate with this particular collapse (Vanderveken 2013).
- All other palatal, oropharynx, and hypopharynx collapse configurations are eligible.
- Complete concentric palatal collapse (see Figure 4) occurs in up to 24% of patients evaluated by DISE and is ineligible for HNS as studies have demonstrated a very low success rate with this particular collapse (Vanderveken 2013).
- < 25% Central + Mixed Sleep Apnea (i.e. at least 75% of apneic episodes detected by sleep study need to be obstructive in nature).
- BMI < 32-35 (depending on the patient's insurance coverage)
- Patient selection is important to optimize results with HNS.
- One study demonstrated a success rate of only 30% in non-selected OSA patients who undergo HNS, highlighting the importance of patient selection (Babtista 2019).
- Recent studies have looked at refining the above criteria.
- A study with 20 pediatric patients with Downs syndrome and OSA treated with HNS showed a similar success rate (mean AHI reduction of 85%) as seen in the adult trials (Caloway 2020).
- Further studies are needed to include the pediatric population in inclusion criteria, however these results are promising.
- Current contraindications found not to be associated with worse patient outcomes: AHI > 65 and previous OSA surgery (Babtista 2020).
- Disorders found to be statistically associated with worse patient outcomes: tongue malformations/palsy, neuromuscular disorders, and positional OSA (Babtista 2020).
- Future studies are looking at including patients with higher BMI.
- A study with 20 pediatric patients with Downs syndrome and OSA treated with HNS showed a similar success rate (mean AHI reduction of 85%) as seen in the adult trials (Caloway 2020).
Nursing Considerations
- Instrumentation and Equipment
- Standard Oto major tray
- Oto microsurgery instrumentation tray
- Vessel loops
- Malleable retractors (thinnest ~ 1 cm retractor is required). Large Rich retractor needed for sense lead placement.
- Operating microscope is required for hypoglossal nerve dissection
- A sterile sleeve is required for the telemetry unit on the field to test the device
- Medtronic NIM nerve monitoring system is required for monitoring of hypoglossal nerve
- Inspire pulse generator #3028, stimulation lead #4063, sense lead #4340
- Medtronic tunneler, MDT Catheter passer (single use), 38 cm, ref 8591-38
- Sutures: 2.0 and 3.0 permanent silk sutures. 3.0 vicryl and 3.0 monocryl for closure
- Equipment required "off the field":
- Bipolar stimulation electrodes x 2 (Xomed 8227304 and 8225401)
- Debakey forceps to grasp and insert the electrodes
- 4x4 gauze to grasp the tongue
- Marker
- Local anesthetic (lidocaine)
- No Foley catheter used
- Positioning:
- Arms tucked (optional)
- Shoulder roll (optional)
- Head turned to right
- Prep and drape (see Figure 5)
- Prep from lower lip, down neck, to xiphoid process with 10% providone iodine
- Drape:
- Square off field with sterile towels
- Place Ioban drape starting at the angle of mandible, down across the chest
- Place 1010 sticky drape along the mandible and up over the mouth so the tongue can be visualized intraoperatively but is separate from the sterile field
- Oto split drape
Anesthesia Considerations
- Preoperative antibiotics (ancef) given within 60 minutes of incision
- Standard orotracheal intubation
- ETT taped to contralateral side of implant
- If needed for intubation, use only short-acting muscle relaxants (avoid long-acting muscle relaxants so hypoglossal nerve can be tested)
- Ipsilateral arm preferentially free of IV, BP cuff, and pulse oximeter
- Ipsilateral chest free of EKG electrodes
- Positioning:
- Turn bed 180 degrees to the left after intubation so that anesthesia is at the foot of the bed
Operative Procedure and Postoperative Care
- No monopolar cautery is used
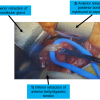
- Patient preparation (see Figure 6)
- Plan neck incision for stimulation electrode: 4-6 cm in length, 1 cm from midline, midway between the hyoid and mandible
- Plan implantable pulse generator and sensor lead incision: midway between the second and third rib beginning 3 cm lateral to the lateral edge of the sternum.
- Incision is a total of 5 cm in length.
- Place NIM electrodes in tongue: grip tongue with gauze and use debakey forceps to place red electrodes very superficially in hyoglossus (ventrolateral tongue 4 cm from tip) and blue electrode in genioglossus (lateral to frenulum and anterior to duct) (see Figure 1)
- Prep and drape as described above
- Neck dissection (see Figure 7)
- Divide skin and platysma to make a small inferior subplatysmal flap
- Take care to avoid injury to the marginal mandibular branch of the facial nerve
- Free up the anterior-inferior portion of submandibular gland and retract in a postero-superior manner
- Identify and retract digastric tendon inferiorly with vessel loops
- Identify the posterior border of mylohyoid and divide ranine vein as necessary
- Retract mylohyoid anteriorly
- Divide skin and platysma to make a small inferior subplatysmal flap
- Hypoglossal nerve identification: place vessel loop to isolate nerve
- Hypoglossal nerve dissection and isolation
- Bring in microscope
- Identify functional breakpoint of hypoglossal nerve using NIM stimulator and neuroanatomy
- Focused nerve dissection at functional breakpoint
- Remap with NIM to confirm breakpoint
- Place stimulator lead around inclusion branches of the hypoglossal nerve (see Figure 8)
- Secure with silk anchor sutures
- IPG (implantable pulse generator) pocket:
- Divide skin and subcutaneous tissue under the 5.5-6 cm chest incision
- Bluntly dissect directly down to pectoralis fascia
- Size pocket to 3 fingerbreadths
- Can optionally place silk retention suture in fascia for later use with IPG
- Sensor lead placement
- Use same chest incision
- Dissect through pectoralis major muscle and anterior serratus muscle if needed. Place large Rich retractor for retraction.
- Deep to the pectoralis major muscle is a fat pad that needs to be carefully divided
- Identify external intercostals (fibers transverse superior-lateral to inferior-medial)
- Carefully dissect through the thin external intercostal muscle 1 cm from its medial edge
- Place 1 cm bent malleable retractor under external intercostal to identify internal intercostal muscle (fibers transverse inferior-lateral to superior-medial)
- Retractor should meet no resistance at it enters the correct plane between internal and external intercostal muscles parallel to the rib space
- Carefully place sensor lead between external and internal intercostal muscles and secure with silk anchor sutures to the medial external intercostal muscle fibers
- Tunneling
- Pass tunneling device from neck incision to IPG pocket in chest, deep to platysma but over the clavicle (this is facilitated by a > 90 bend on tunneler). Then pass stimulator lead through the neck tunnel into IPG pocket.
- Ensure adequate excess lead at both ends of tunnel to prevent device tethering.
- Connect leads to IPG
- Place IPG in pocket and secure using 2 air knots
- Make sure leads are lying flat to prevent extrusion
- Test device
- Monitor tongue movement during testing to ensure tongue protrusion and absence of retraction or depression.
- Ensure good respiration sensing signal from sensing lead
- Closure
- Establish hemostasis and then irrigate the surgical sites
- Neck incision: 3-0 vicryl deep, 4-0 monocryl superficial, dermabond
- Chest incision: 3-0 vicryl deep, 4-0 monocryl superficial, dermabond
- Pressure dressings placed over incision
- Pre-discharge:
- Obtain postoperative x-ray
- Standard chest AP to visualize pulse generator, stimulating, and sensing electrode
- Lateral neck to visualize stimulating electrode
- Diet: general when patient is alert
- Same day discharge or overnight observation
- Obtain postoperative x-ray
- Antibiotics: (Keflex) for 1 week (optional)
- Activity:
- Avoid strenuous activities for 4 weeks
- Follow-ups:
- 1-2 days to assess tongue movement, inspect incisions, and remove dressings.
- 4 weeks for initial device activation
- 3-4 months for polysomnogram and fine-tuning device titration.
- Device titration allows for precision medicine by maximizing efficacy while mitigating side effects. Can be adjusted over time as needed by patient or provider.
Dictation Template
-
The patient was brought to the Operating Room and was anesthetized via general endotracheal anesthesia without complication. A shoulder roll was placed and the patient was prepped and draped in usual sterile fashion with the head turned to the left. Prior to prepping and draping, electrodes were placed in the genioglossus and hyoglossus muscles and connected to the NIM box for intraoperative nerve monitoring.
A modified sub-mandibular incision was made in the right upper neck approximately 2 cm below the mandible in the natural skin crease. Dissection was carried down through the subcutaneous tissue and platysma. The anteroir-inferior border of the submandibular gland was identified as well as the digastric tendon. The submandibular gland and the overlying fascia with the marginal mandibular nerve were retracted superiorly. The digastric tendon was retracted inferiorly. Dissection was carried down into the digastric triangle where the hypoglossal nerve was identified in its usual position. The mylohyoid muscle was retracted anteriorly, and the hypoglossal nerve was dissected up towards the floor of the mouth. The lateral branches to retrusor muscles were identified and tested intra-operatively using the NIM stimulator. The cuff electrode for the hypoglossal nerve stimulator (C1778; L8680) was placed distally to these branches on the medial nerve branch to the genioglossus muscle. Diagnostic evaluation confirmed activation of the genioglossus nerve, resulting in genioglossal activation and tongue protrusion, confirmed visually.
A second 5-6 cm incision was made in the right upper chest approximately 3 cm below the clavicle. Dissection was carried down to the pectoralis muscle. An inferior pocket was created deep to the subcutaneous layer and superficial to the pectoralis muscle. The stimulation electrode was then looped under and secured to the digastric tendon on its lateral surface with the provided anchor. The stimulation lead was then tunneled in a subplatysmal plane and brought out into the sub-clavicular pocket.
Through the same chest incision, dissection was carried down through pectoralis major muscle. The external oblique muscles were identified, and incised, and a tunnel was created between the external and internal intercostals in the third intercostal space just on the superior aspect of the fourth rib. The pleural respiration sensor (C1778; L8680) was placed into the pocket in the inferior aspect of the third intercostal space. The sensor was sutured to the fascia using the provided anchors to maintain the sensor facing the pleural space. Both the cuff electrode and the respiration sensing lead were connected to the implantable pulse generator in the pectoralis fascia pocket. Diagnostic evaluation was again run, which confirmed a good respiration sensing signal as well as good tongue protrusion and no tongue retraction with stimulation.
The implantable pulse generator (C1767; L8688) was placed in the subclavicular pocket and secured loosely to the pectoralis fascia using non-resorbable sutures. All the wounds were thoroughly irrigated with bacitracin irrigation. The wounds were then closed in three layers with deep Polysorb sutures and a 4-0 running subcuticular monocryl. Dermabond was applied followed by pressure dressings.
The patient was then awakened, extubated, and transferred to recovery room in stable condition.
References
Baptista PM, Costantino A, Moffa A, Rinaldi V, Casale M. Hypoglossal Nerve Stimulation in the Treatment of Obstructive Sleep Apnea: Patient Selection and New Perspectives. Nat Sci Sleep. 2020 Feb 13;12:151-159. doi: 10.2147/NSS.S221542. PMID: 32104122; PMCID: PMC7026121.
Costantino A, Rinaldi V, Moffa A, Luccarelli V, Bressi F, Cassano M, Casale M, Baptista P. Hypoglossal nerve stimulation long-term clinical outcomes: a systematic review and meta-analysis. Sleep Breath. 2020 Jun;24(2):399-411. doi: 10.1007/s11325-019-01923-2. Epub 2019 Aug 15. PMID: 31418162.
Gottlieb DJ, Punjabi NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA. 2020;323(14):1389–1400. doi:10.1001/jama.2020.3514
Woodson BT, Strohl KP, Soose RJ, Gillespie MB, Maurer JT, de Vries N, Padhya TA, Badr MS, Lin HS, Vanderveken OM, Mickelson S, Strollo PJ Jr. Upper Airway Stimulation for Obstructive Sleep Apnea: 5-Year Outcomes. Otolaryngol Head Neck Surg. 2018 Jul;159(1):194-202.
Van Daele DJ, Cromwell JW, Hsia JK, Nord R. Post-operative complication rate comparison between airway surgery and upper airway stimulation using NSQIP and ADHERE. OTO Open. Accepted for publication 9/1/2021.
Eastwood PR, Barnes M, MacKay SG, Wheatley JR, Hillman DR, Nguyên XL, Lewis R, Campbell MC, Pételle B, Walsh JH, Jones AC, Palme CE, Bizon A, Meslier N, Bertolus C, Maddison KJ, Laccourreye L, Raux G, Denoncin K, Attali V, Gagnadoux F, Launois SH. Bilateral hypoglossal nerve stimulation for treatment of adult obstructive sleep apnoea. Eur Respir J. 2020 Jan 9;55(1):1901320. doi: 10.1183/13993003.01320-2019. PMID: 31601716; PMCID: PMC6949509.
Byun YJ, Yan F, Nguyen SA, Lentsch EJ. Transcutaneous Electrical Stimulation Therapy in Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. Otolaryngol Head Neck Surg. 2020 Oct;163(4):645-653. doi: 10.1177/0194599820917631. Epub 2020 May 5. PMID: 32366179.
Ratneswaran D, Guni A, Pengo MF, Al-Sherif M, He B, Cheng MC, Steier J, Schwarz EI. Electrical stimulation as a therapeutic approach in obstructive sleep apnea - a meta-analysis. Sleep Breath. 2021 Mar;25(1):207-218. doi: 10.1007/s11325-020-02069-2. Epub 2020 May 9. PMID: 32388780.
Neruntarat C, Wanichakorntrakul P, Khuancharee K, Saengthong P, Tangngekkee M. Upper airway stimulation vs other upper airway surgical procedures for OSA: a meta-analysis. Sleep Breath. 2021 May 17. doi: 10.1007/s11325-021-02402-3. Epub ahead of print. PMID: 33999362.
Kent DT, Scott WC, Zealear D, Schwartz AR. Ansa cervicalis stimulation increases pharyngeal patency in patients with obstructive sleep apnea. J Appl Physiol (1985). 2021 Aug 1;131(2):487-495. doi: 10.1152/japplphysiol.00076.2021. Epub 2021 Jul 1. PMID: 34197226.
Clemens Heiser, Armin Steffen, Maurits Boon, Benedikt Hofauer, Karl Doghramji, Joachim T. Maurer, J. Ulrich Sommer, Ryan Soose, Patrick J. Strollo Jr, Richard Schwab, Erica Thaler. Post-approval upper airway stimulation predictors of treatment effectiveness in the ADHERE registry. European Respiratory Journal 2019 53: 1801405
Baptista PM, Costantino A, Moffa A, Rinaldi V, Casale M. Hypoglossal Nerve Stimulation in the Treatment of Obstructive Sleep Apnea: Patient Selection and New Perspectives. Nat Sci Sleep. 2020 Feb 13;12:151-159. doi: 10.2147/NSS.S221542. PMID: 32104122; PMCID: PMC7026121.
Caloway CL, Diercks GR, Keamy D, de Guzman V, Soose R, Raol N, Shott SR, Ishman SL, Hartnick CJ. Update on hypoglossal nerve stimulation in children with down syndrome and obstructive sleep apnea. Laryngoscope. 2020 Apr;130(4):E263-E267. doi: 10.1002/lary.28138. Epub 2019 Jun 20. PMID: 31219619.
Parikh V, Thaler E, Kato M, Gillespie MB, Nguyen S, Withrow K, Calhoun D, Soose R, Stevens D, Stevens S, Larsen C, Reddy M, Lakkireddy D. Early feasibility of hypoglossal nerve upper airway stimulator in patients with cardiac implantable electronic devices and continuous positive airway pressure-intolerant severe obstructive sleep apnea. Heart Rhythm. 2018 Aug;15(8):1165-1170. doi: 10.1016/j.hrthm.2018.04.016. Epub 2018 Apr 18. PMID: 29678782.
Vanderveken OM, Maurer JT, Hohenhorst W, Hamans E, Lin HS, Vroegop AV, Anders C, de Vries N, Van de Heyning PH. Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. J Clin Sleep Med. 2013 May 15;9(5):433-8. doi: 10.5664/jcsm.2658. PMID: 23674933; PMCID: PMC3629316.
Safiruddin F, Vanderveken OM, de Vries N, Maurer JT, Lee K, Ni Q, Strohl KP. Effect of upper-airway stimulation for obstructive sleep apnoea on airway dimensions. Eur Respir J. 2015 Jan;45(1):129-38. doi: 10.1183/09031936.00059414. Epub 2014 Sep 3. PMID: 25186270.