Return to: Salivary Duct Stenosis (or click for more detail: Etiology / Diagnosis / Management); Anatomy of submandibular gland and duct
University of Iowa Sialogram Classification (Grading Scale)
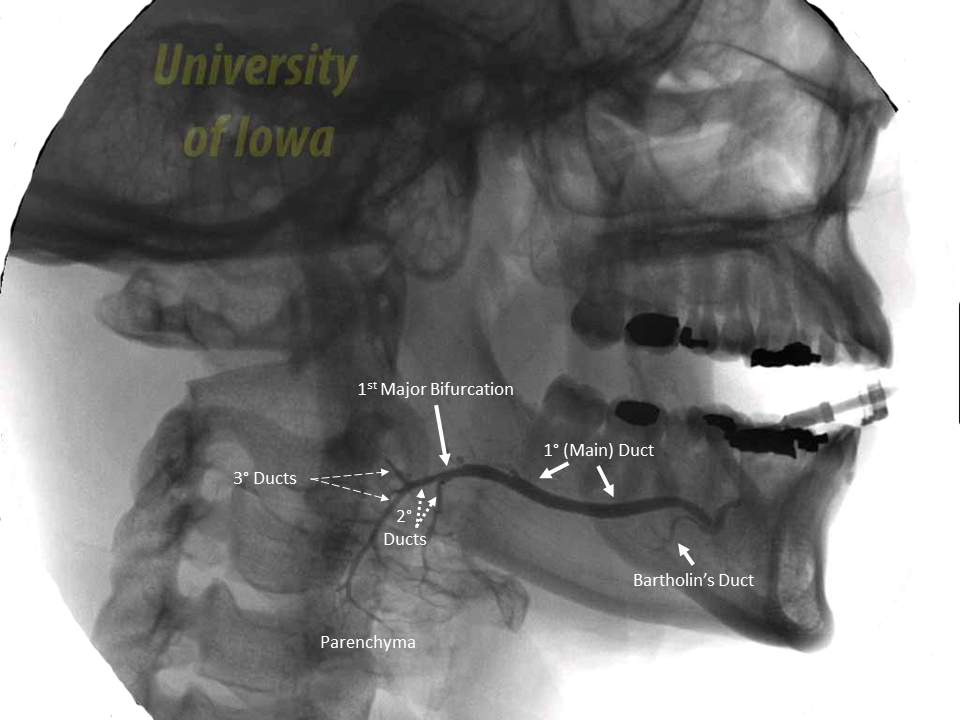
Addressing Ductal Stenosis - adaptable for Parotid and Submandibular Sialograms
1º (main duct): segment of duct from the oral cavity to the first major bifurcation
2º (secondary): segment of duct proximal to first major bifurcation and distal to second bifurcation
3º (tertiary): any duct proximal to the second bifurcation (including those that could be considered quaternary)
Scoring system adapted from Foggia et al (Foggia 2020), Thorpe et al (Thorpe 2020), and Blatt et al (Blatt 1956)
Score |
Location of Stenosis(diagram below) |
Degree of Stenosis |
Retention of Contrast |
Peripheral Duct Dilation |
|
0 |
No stenosis |
No stenosis |
None |
None |
|
1 |
Tertiary or quaternary duct |
Minimal <25% stenotic |
Focal retention pockets |
Punctate dilation < 1 mm diamter |
|
2 |
Secondary duct |
Mild 25-50% stenotic |
Indistict retention |
Globular dilation 1-2 mm diameter |
|
3 |
Main duct |
Moderate 50-75% stenotic |
N/A |
Coalescent irregularly shaped globules > 2mm diameter |
|
4 |
N/A |
Severe >75% stenotic |
N/A |
Destructive of gland parenchyma |
Classification Systems based on sialendoscopy findings:
A. Koch et al (Koch 2008, Koch 2009, Koch 2012, Koch 2020) - Stensen's duct stenosis (Koch et al 2009) based on sialendoscopy evaluation of tissue quality / luminal narrowing, extet, number, location and considerations for etiology
Type I: Inflammation dominated with variable narrowing of the lumen; slight fibrotic remodeling; obstructive plaques
Type II: Fibrotic stenosis, often short segment and web-associated, predominant incomplete (luminal narrowing <50%); circular or web-like encroachments of the duct wall, megaduct
Type III: Fibrotic stenosis, massive fibrotic reaction of the duct wall - predominantly high-grad luminal narrowing >50%
B. Kopec et al 2013 (Kopec 2013) proposal for classification of stenoses of Wharton's duct based on site of stenosis - which they also applied to Stensen's duct
Based on evaluation via sialendoscopy (done under local anesthesia with 1.0 to 1.6 mm modular semirigid sialendoscopes) of stenosis of submandibular gland (24 patients) and parotid gland (27 patients)
'A stenosis was diagnosed when the duct was not passable with the 1.0 mm sialoendoscope and with additional instrumental dilatation'
Kopec et al (Kopec 2013) employed a Modification of Koch et al classification (Koch 2008, Koch 2009) dividing ducts into three parts
Determined by measurements during sialendoscopy (mentioned it was possible due to shaft of sialoendoscope marked in cm)
|
Kopec et al 2013 Ductal Stenosis Classification |
Parotid (Stensen's Duct) |
Submandibular (Wharton's Duct) |
| 1st segment |
Papilla up to 1 cm (before passing through the buccinator) |
Papilla up to 1 cm |
| 2nd segment |
Middle (area of buccinator to 2 cm behind it) |
Middle (between 2 and 4 cm) |
| 3rd segment | Hilum |
Proximal (from 1 cm before the hilum up to the hilar system) |
Papilla/distal
Middle
Proximal/hilum
Diffuse
C. Marchal et al (Marchal 2007, 2008, 2009)
Classification based on site of stenosis (main or accessory duct), extent and number (adapted from Kopec 2013 referring for French publication Marchal 2009)
Marchal 2007: Classified strictures of both parotid and submandibular glands into 4 types
Adapted from Marchal (2009) |
Description |
Comment |
| Type I | Membranous stricture | thin/localized - usually in second and higher generation branches |
| Type II | Large stricture | less than 1 cm - usually affecting main duct |
| Type III | Diffuse stenosis of main duct | normal intraglandular ductal system |
| Type IV (a/b) | Diffuse generalized stenosis | affecting whole ductal system |
| Type IV a | Diffuse generalized stenosis without localized strictures | diffuse reduction of caliber without other strictures |
| Type IV b | Diffuse generalized stenosis with multiple localized strictures | diffuse reduction of caliber associated with irregular strictures |
Marchal et al (Marchal 2008) "L-S-D" Classification (L = Lithiasis; S = Stenosis; D = Endoscopic Classification of Dilatation)
L0= Duct free of stone; L1= Floating stone; L2= Fixed stone, totally visible (L2a < 8mm / L2b > 8mm); L3 Fixed stone partially visible (L3a palpable / L3b not palpable)
S0= No stenosis; S1= Intraductal Diaphragmatic stenosis (may be multiple); S2= Unique ductal stenosis (main duct); S3 Multiple of diffuse ductal stenosis (main duct); S4 Generalized ductal
D0= No dilatation; D1 Unique; D2 Multiple; D3 Generalized
D. Ngu et al (Ngu 2007)
Dental Radiology Department (London teaching hospital); salivary duct stricture defined: "a narrowing of the duct to such a degree as to cause impairment or obstruction to the normal smooth out-flow of saliva"
Classified as single or multiple affecting zones: 'anterior third'; 'middle third'; 'posterior third including hilum'
10 year (ending 2004) retrospective study of all patients identifying 1,362 sialograms performed on patients with 'obstructive symptoms': 877 (64.4%) with sialographic findings of benign intradcutal obstruction (485 were normal)
- 642/877 (73.2%) due to salivary calculi
- 198/877 (22.6%) 'ductal strictures as the primary cause of obstruction
- 37/877 (4.2%) mucous plugs
Single strictures 132 (66.7%); Multiple strictures 66 (33.3%); most common site for parotid was middle third (41%); most common site for submandibular was posterior third/hilum
Sialogram technique: 'patient upright in dental chair with three radiographs taken of the lgand using and intraoral X-ray tube - two oblique lateral views and one anteroposterior radiograph - then reviewed in darkened room by transmitted light and with a x2 magnification available.
References
Thorpe RK, Foggia MJ, Marcus KS, Policeni B, Maley JE, Hoffman HT. Sialographic Analysis of Radioiodine-Associated Chronic Sialadenitis. Laryngoscope. 2020 Nov 17. doi: 10.1002/lary.29279. Epub ahead of print. PMID: 33200832.
Foggia MJ, Peterson J, Maley J, Policeni B, Hoffman HT. Sialographic analysis of parotid ductal abnormalities associated with Sjogren's syndrome. Oral Dis. 2020 Jul;26(5):912-919. doi: 10.1111/odi.13298. Epub 2020 Mar 3. PMID: 32031309.
Truong K, Hoffman HT, Policeni B, Maley J. Radiocontrast Dye Extravasation During Sialography. Ann Otol Rhinol Laryngol. 2018 Mar;127(3):192-199. doi: 10.1177/0003489417752711. Epub 2018 Jan 7. PMID: 29308655.
Choi JS, Choi YG, Kim YM, Lim JY. Clinical outcomes and prognostic factors of sialendoscopy in salivary duct stenosis. Laryngoscope. 2018 Apr;128(4):878-884. doi: 10.1002/lary.26897. Epub 2017 Oct 8. PMID: 28988448.
Blatt, I. M., French, A. J., Holt, J. F., Maxwell, J. H., & Rubin, P. (1956). Secretory sialography in diseases of the major salivary glands. The Annals of Otology, Rhinology, and Laryngology, 65(2), 295–317. https:// doi.org/10.1177/000348945606500201
Koch M, Iro H, and Zenk J: Sialendoscopy-based diagnosis and classification of parotid duct stenosis. Laryngoscope 2009 Sep;119(9):1696-703
Kopec T, Szyfter W, Wierzbicka M, and Nealis J: Stenoses of the salivary ducts-sialendoscopy based diagnosis and treatment. British Journal of Oral and Maxillofacial Surgery Volume 51, Issue 7, October 2013
Koch M, Iro H, Kunzel J, Psychogios G, Bozzato A, and Zenk J: Diagnosis and gland-preservjng minimally invasive therapy for Wharton's duct stenoses. Laryngoscope 122 (2012) pp 552-558
Koch M, Iro H, Zenk J. Role of Sialoscopy in the Treatment of Stensen’s Duct Strictures. Annals of Otology, Rhinology & Laryngology. 2008;117(4):271-278. doi:10.1177/000348940811700406
Marchal F, C. Chossegros, F. Faure, B. Delas, A. Bizeau, B. Mortensen, et al.Publié Sous l’Egide de la Société Européenne des Glandes Salivaires, Salivary stones and stenosis. A comprehensive classification (in French)
Rev Stomatol Chir Maxillofac, 110 (2009), pp. 1-4
Ngu RK, Brown JE, Whaites EJ, Drage NA, Ng SY, Makdissi J. Salivary duct strictures: nature and incidence in benign salivary obstruction. Dentomaxillofac Radiol. 2007 Feb;36(2):63-7. doi: 10.1259/dmfr/24118767. PMID: 17403881.
Koch M, Zenk J, Iro H. Stenosis and stenosis-like lesions in the submandibular duct: Detailed clinical and sialendoscopy-based analysis and proposal for a classification. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020 Nov;130(5):486-495. doi: 10.1016/j.oooo.2020.05.015. Epub 2020 Jun 5. PMID: 32665204.
Marchal F Chapter 6 Sialendoscopy pp 128-145 in Salivary Gland Disorders eds Myers EN and Ferris RL Springer-Verlag Berlin Heidelberg 2007
Marchal F, Chossegros C, Faure F, Delas B, Bizeau A, Mortensen B, Schaitkin B, Buchwald C, Cenjor C, Yu C, Campisi D, Eisele D, Greger D, Trikeriotis D, Pabst G, Kolenda J, Hagemann M, Tarabichi M, Guntinas-Lichius O, Homoe P, Carrau R, Irvine R, Studer R, Wang S, Fischer U, Van der Poorten V, Saban Y, Barki G. Salivary stones and stenosis. A comprehensive classification. Rev Stomatol Chir Maxillofac. 2008 Sep;109(4):233-6. doi: 10.1016/j.stomax.2008.07.004. Epub 2008 Sep 5. PMID: 18774150.
