Iowa Thoracic Surgery Protocols
Albert Pai, MD, John C. Keech, MD, Mohamad Bashir, MD, Melissa Tvedte, ARNP, Kalpaj R. Parekh, MBBS, Evgeny V. Arshava, MD
Please direct questions and comments to Evgeny V. Arshava, MD evgeny-arshava@uiowa.edu
See also other sections on Thoracic Surgery
Thoracic duct: anatomy and physiology. Chylothorax: diagnosis and management.
GENERAL CONSIDERATIONS
Esophageal diverticula are categorized based on their anatomic location along the esophagus and whether they are pulsion (false) or traction (true) diverticula. Diverticula of the esophagus can be located at any level with the most common anatomic presentations occurring at the cervical, the mid-thoracic, and the epiphrenic region.
Pharyngoesophageal (Zenker’s) diverticulum is a pulsion diverticulum predictably located in the cervical esophagus at the level of the pharynx through the Killian’s triangle, bordered by the cricopharyngeus distally and thyropharyngeus (part of inferior pharyngeal constrictor) muscles. It will not be discussed on this page section (see: Zenker's Diverticulectomy).
The diverticular of the esophageal body (mid-esophageal and epiphrenic) can be either pulsion or traction. Midesophageal diverticula are confined within the mid-1/3 of the esophagus approximately 5 cm above and 5 cm below the carina.
Epiphrenic esophageal diverticula are located within 10 cm above the GEJ. They commonly develop on the right posterolateral side of the esophageal wall and are associated with a small sliding hiatal hernia. Both of these types are uncommon and collectively account for 30% of esophageal diverticula.
The distinction between pulsion and traction diverticula relates to the mechanism of pathology. Pulsion diverticula may reach sizable dimensions, occur due to an increase in intraluminal pressure (usually secondary to an esophageal motility disorder), which causes herniation of mucosal and submucosal layers. Traction diverticula tend to be smaller and occur due to external traction of the esophageal wall from chronic mediastinal inflammation (such as from tuberculosis or histoplasmosis lymphadenopathy). As a result of an external traction force, an outpouching will form with all three mucosal, submucosal, and muscular layers of the esophageal wall. Mid-esophageal diverticula (area that corresponds to the packet of larger subcarinal nodes and hence frequently called "subcarinal") are almost exclusively traction type, and epiphrenic diverticula are usually pulsion type.
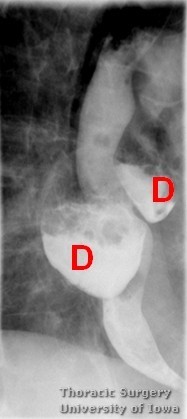
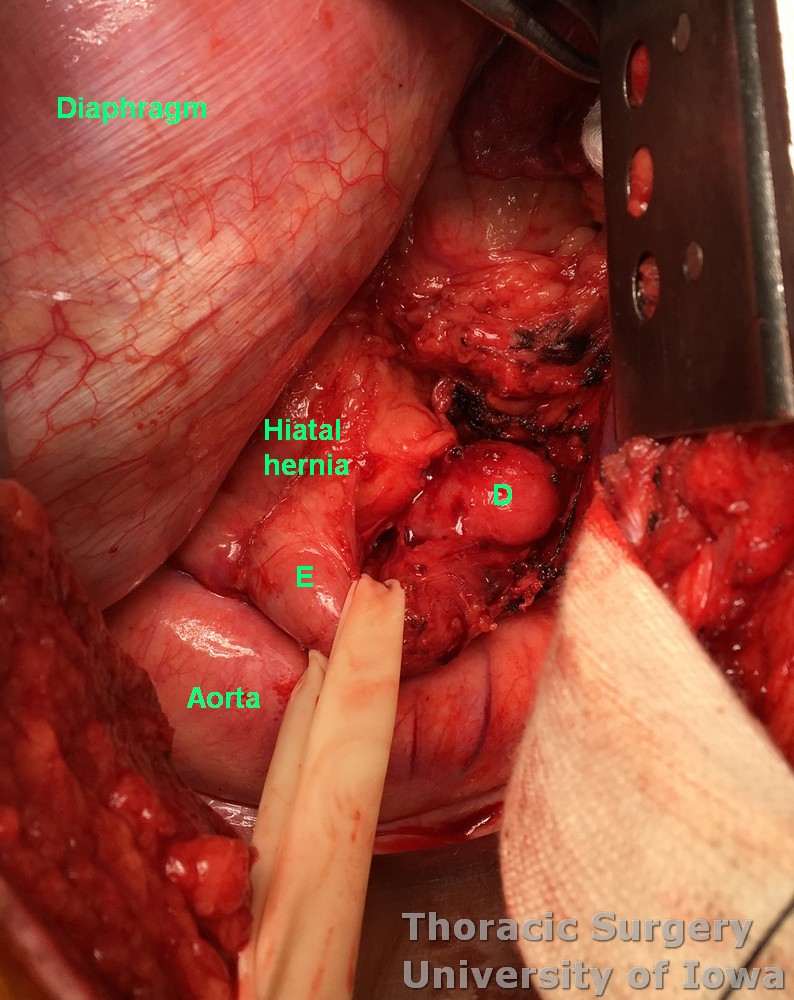
Pulsion diverticula (D - on image below) can occasionally be multiple and located on different levels of the esophagus.
Both traction and epiphrenic diverticula are largely asymptomatic. Symptoms typically develop in a diverticulum above 5 cm in width (typically pulsion) including aspiration, regurgitation, and esophageal luminal compression from the diverticular pouch. A diverticulectomy is thus warranted for symptomatic relief. At the University of Iowa, our preferred approach is a posterolateral thoracotomy, stapled diverticular resection, and esophageal myotomy. The importance of esophageal myotomy for pulsion diverticula is essential to prevent recurrence of diverticulum and decrease the risk of diverticulectomy site leak.
Traction diverticula more commonly present with infection complications. Ongoing inflammation that caused them may result in full thickness erosion through the esophageal wall with esophagobronchial fistulas, mediastinitis and other complications. Surgical interventions for these are typically tailored to address complications.
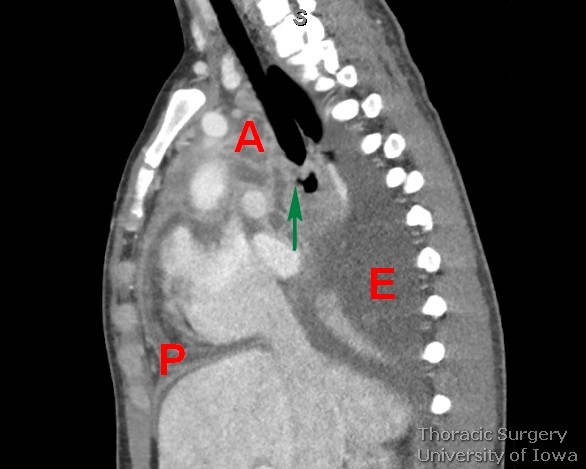
Below is a chest CT image of a perforated traction diverticulum (arrow) resulting in a multiloculated mediastinal abscess (A), purulent pericarditis (P) and pleural effusion (E).
INDICATIONS
-
Symptomatic diverticulum (dysphagia, food regurgitation, substernal chest pain, weight loss, recurrent aspiration)
-
Complications related to the diverticulum (bronchial, pleural, or aortic fistulae)
-
Progression in size of the diverticulum
CONTRAINDICATIONS
-
Asymptomatic patient
-
Associated medical comorbid conditions
PERTINENT ANATOMY
Approaches to the esophagus
-
Upper and middle thoracic esophagus is located behind trachea, carina, and left atrium. The azygos vein courses over this portion of the esophagus. The aorta ascends along left side of the esophagus and supplies it with several esophageal branches.
-
Lower thoracic esophagus (as it courses to the left) and esophageal hiatus may be exposed through the left chest to repair esophageal perforation or reduce diaphragmatic hernia.
Blood supply
-
The upper thoracic esophagus receives branches from the thyroid artery to the level of the tracheal bifurcation, but the majority are derived from arteries arising at the inflection of the aorta.
-
The intraesophageal veins are composed of the subepithelial plexus which is located in the lamina propria. These are arranged longitudinally and extend throughout the entire length of the submucosa.
-
The extraesophageal veins drain into the inferior thyroid veins, the azygos and hemiazygos veins, the left gastric vein, and the splenic vein.
Innervation
-
Vagal nerves are found on both sides of the esophagus. At the gastroesophageal junction (GEJ), the left vagus nerve deviates anteriorly and the right vagus nerve posteriorly as they both descend onto the stomach.
-
Division of bothvagal nerves during esophageal mobilization requires a pylorus-relaxing procedure to facilitate gastric emptying.
-
-
Thoracic duct (See also Thoracic duct: anatomy and physiology. Chylothorax: diagnosis and management) originates at cisterna chyli at the level of L1-2 vertebrae to the right posterior aspect of the aorta. It enters the chest via the aortic hiatus and travels between aorta, esophagus and azygos vein. At the T5 level, it crosses to the left and ascends behind the trachea and the esophagus to the left neck above the clavicle. It drains into the confluence of left subclavian vein with the internal jugular vein.
PREOPERATIVE PREPARATION
Evaluation
Prior to any elective operative therapy, complete work-up for esophageal mechanical obstruction (esophagram), motility disorders (manometry) and GERD (pH manometry) and associated mucosal lesions (endoscopy) must be performed.
-
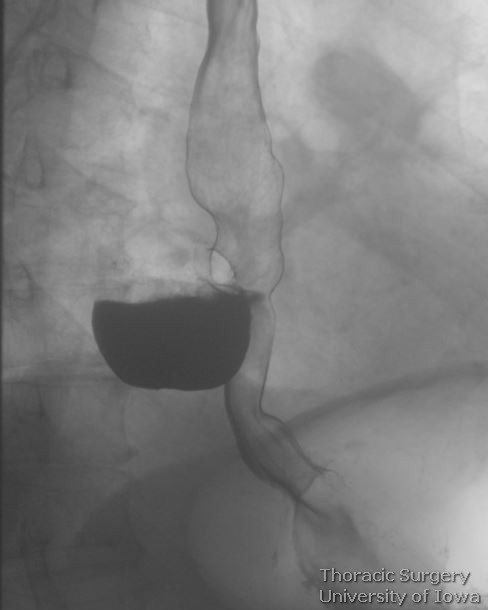
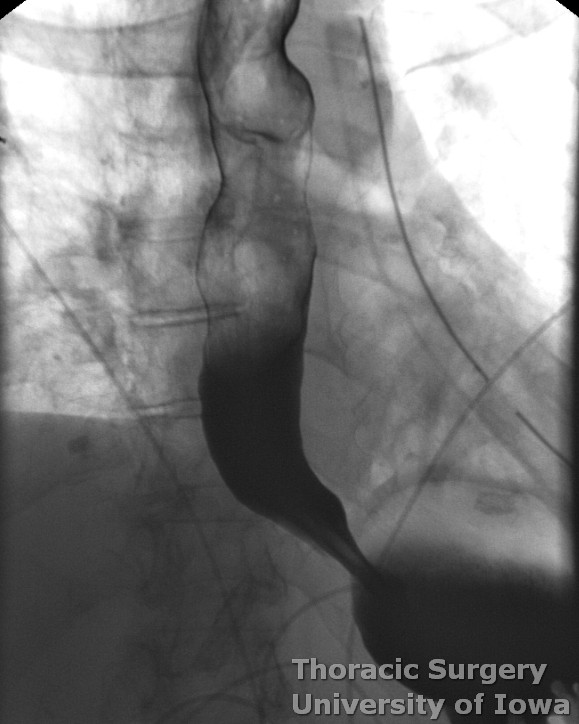
Barium esophagram is typically the first diagnostic test to be performed. This provides diagnostic findings and information useful for surgical planning, including location of the diverticulum (left vs right and distance from diaphragmatic hiatus), the diameter of the pouch, and length and width of its neck. Esophagram may also reveal areas of mechanical obstruction, GEJ abnormalities such as hiatal hernias or lesions suspicious for malignant processes.
-
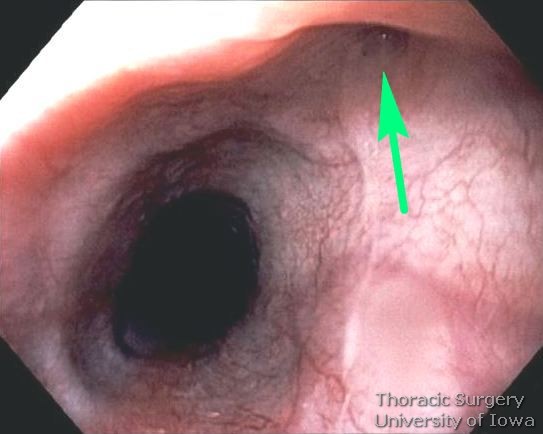
Upper endoscopy assesses the orientation of the diverticulum and evaluates for additional mucosal lesions in the esophagus such as neoplasia, Barrett’s esophagus, esophageal and gastric ulcers.

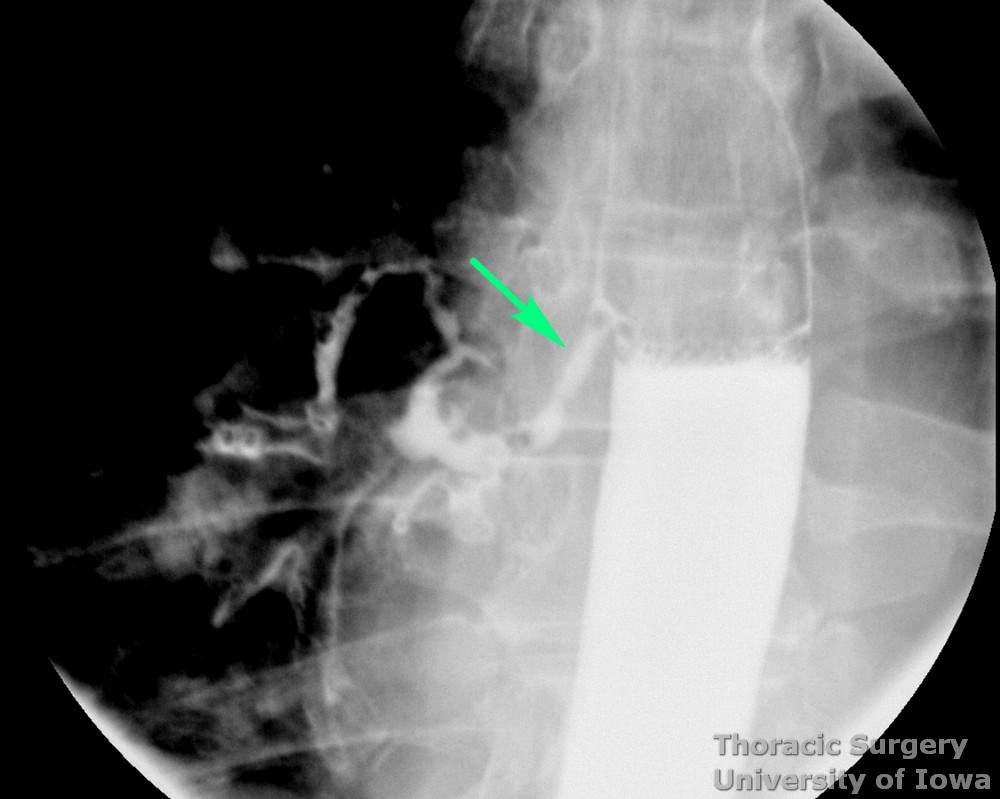
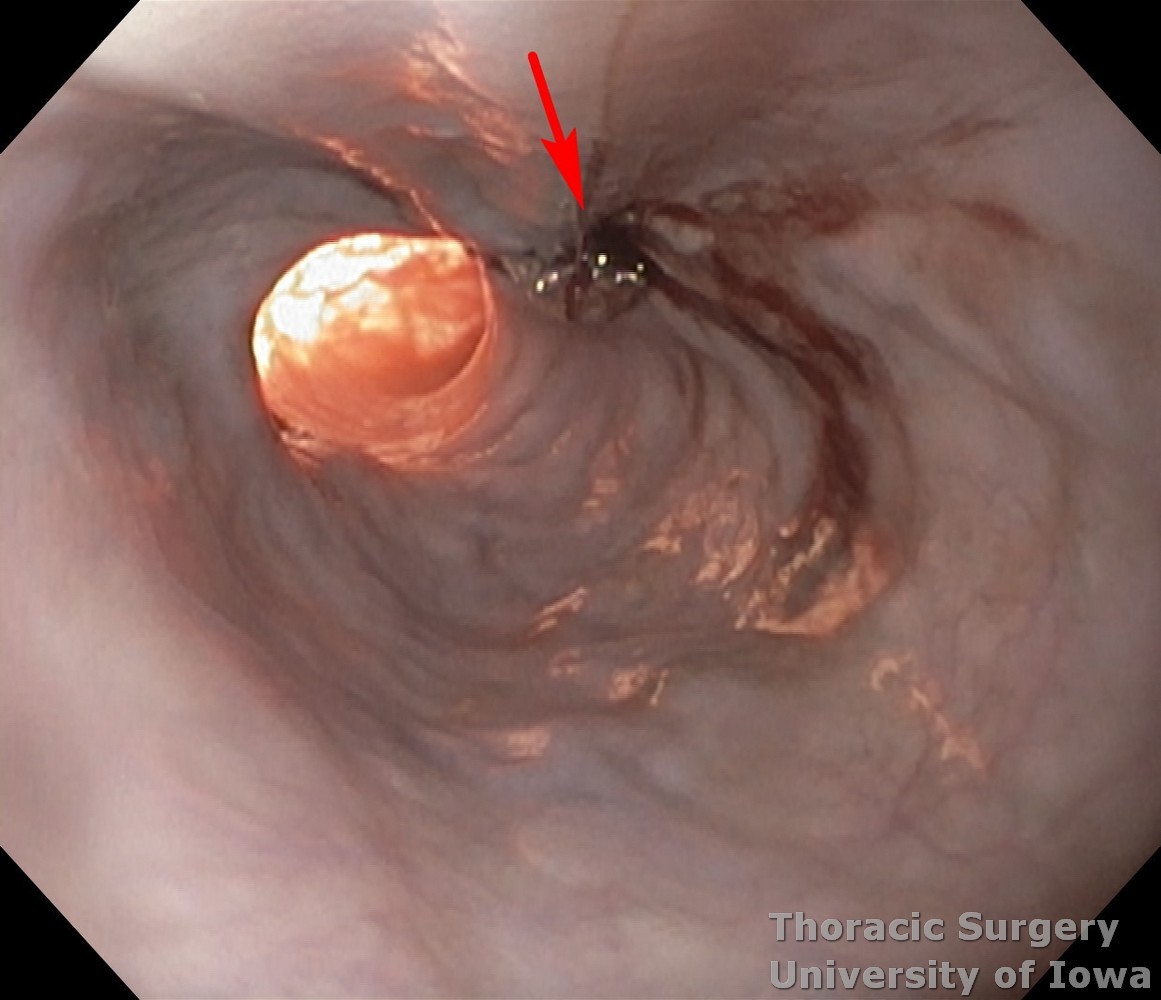
Endoscopic image demonstrating small traction subcarinal diverticulum (arrow) in patient with mediastinal granulomatosis caused by Histoplasma.
-
Esophageal manometry is performed to identify any underlying motility disorders. Commonly associated motility disorders include achalasia, diffuse esophageal spasm, nutcracker esophagus, and hypertensive esophagus. This data allows to decide on the distal extent of myotomy.
-
Computed tomography may further define the anatomy and rule out coexisting unrelated intrathoracic pathology (pulmonary lesions).
-
Ambulatory pH monitoring is not an absolutely necessary step for all esophageal diverticula, but it is used to characterize patients presenting with symptoms such as heartburn and regurgitation to rule out GERD. This is important as the treatment for GERD is diametrically opposite to that of the epiphrenic diverticulum and other motility disorders.
Patient preparation
-
Complete abstinence from smoking for 2-3 weeks prior to operation is of paramount importance just like for any other intrathoracic operation.
-
Nutritional assessment and counseling.
-
Nasogastric/gastrostomy/jejunostomy feeding tube when dysphagia or esophageal obstruction precludes adequate oral calorie intake.
Potential Complications
-
Staple line leak or dehiscence
-
Recurrence of the diverticulum
-
Esophageal stricture
-
Gastroesophageal reflux
-
Aspiration Pneumonitis/Pneumonia
-
Atelectasis
-
Chylothorax
-
Hiatal hernia
-
Injury to the tracheobronchial tree
-
Major bleeding (azygous vein, aorta)
-
Recurrent laryngeal nerve injury
-
Vagus nerve injury
ANESTHESIA CONSIDERATIONS
General
-
Double-lumen endotracheal tube (ETT); single-lumen ETT may be used during EGD phase
-
Epidural catheter placed preoperatively
-
Two large bore peripheral IVs
-
Radial arterial line
-
Central venous line for selected patients only
-
Type and Cross
-
IV antibiotics (Cefazolin) within 1h of the incision (vancomycin within 2h of the incision for b-lactam allergy)
Specific
-
Indwelling Foley catheter
-
Patient initially in supine position for EGD. The flexible endoscope will remain in place during positioning for the thoracic phase.
-
Position in the right lateral decubitus position (for left thoracotomy) with an axillary roll placed 2-3 fingerbreadths below the axilla. The iliac crest is positioned just below the break of the bed.
NURSING CONSIDERATIONS
Instrumentation and Equipment
Standard
-
Flexible esophagogastroduodenoscope (EGD)
-
Weighted Maloney bougie (up to 56 Fr)
-
Major chest stray
-
Energy device (we prefer Ligasure) may be helpful
-
Endoscopic linear cutting stapler
Prep and Drape
-
Standard prep using chlorhexidine solution
-
Field includes:
-
Supraclavicular area to below costal margin; spine to nipple line
-
Drains and Dressings
-
32 Fr angled chest tube
-
16-18 Fr nasogastric tube
OPERATIVE PROCEDURE
EGD phase
-
Single-lumen or double-lumen ETT may be used.
-
Examine the esophageal and gastric mucosa.
-
Retroflex the scope in the stomach to rule-out a hiatal hernia or other pathology.
-
Secure the scope in place with the lights off for positioning for the thoracic phase.
Thoracic phase
-
As most diverticula that require operation epiphrenic, approaches usually through the left chest. Rarely, approach to the right chest may be necessary based on preoperative imaging.
-
While thoracoscopic approach has been described for diverticulectomy and myotomy, it should be limited to select centers and patients.
-
Single-lumen ETT (if used for EGD) is exchanged for double-lumen ETT. The left lung is isolated.
-
Left serratus-sparing posterolateral thoracotomy through the 6th or 7th intercostal space is performed (See section Posteriolateral Thoracotomy). The inferior rib is shingled at the posterior aspect (See Thoracotomy page).
-
Divide the inferior pulmonary ligament to the level of the inferior pulmonary vein.
-
Retract the left lower lobe of the lung anteriorly and superiorly, and depress the diaphragm caudally. Heavy stay stitch may be placed through the dome of diaphragm, to retract it through the future thoracostomy tube site.
-
Incise the mediastinal pleura along the anterior border of the aorta, along the left crus of the diaphragm, and along the posterior pericardial reflection.
-
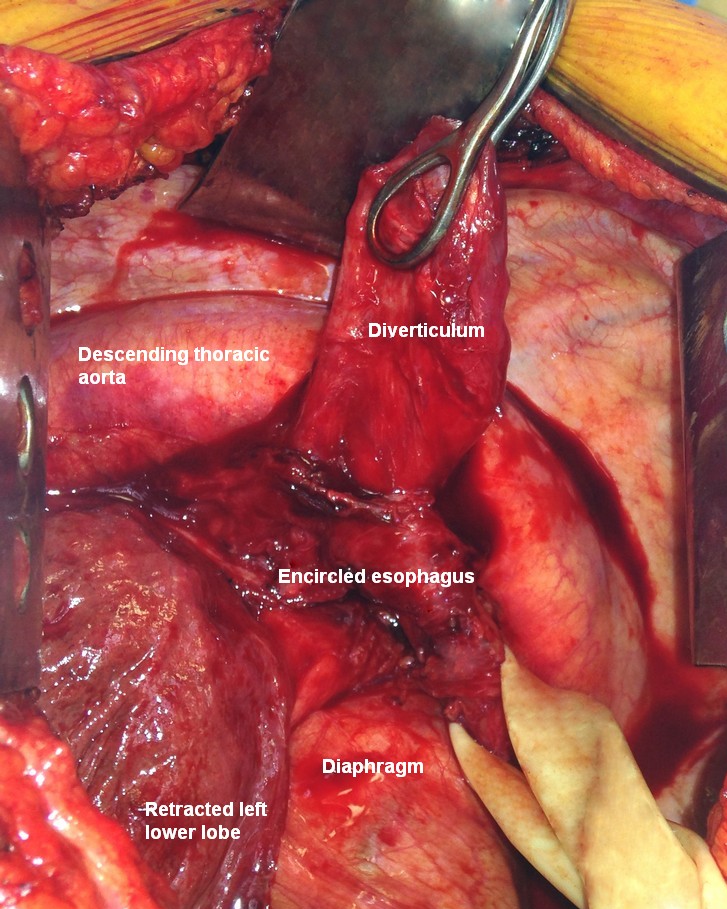
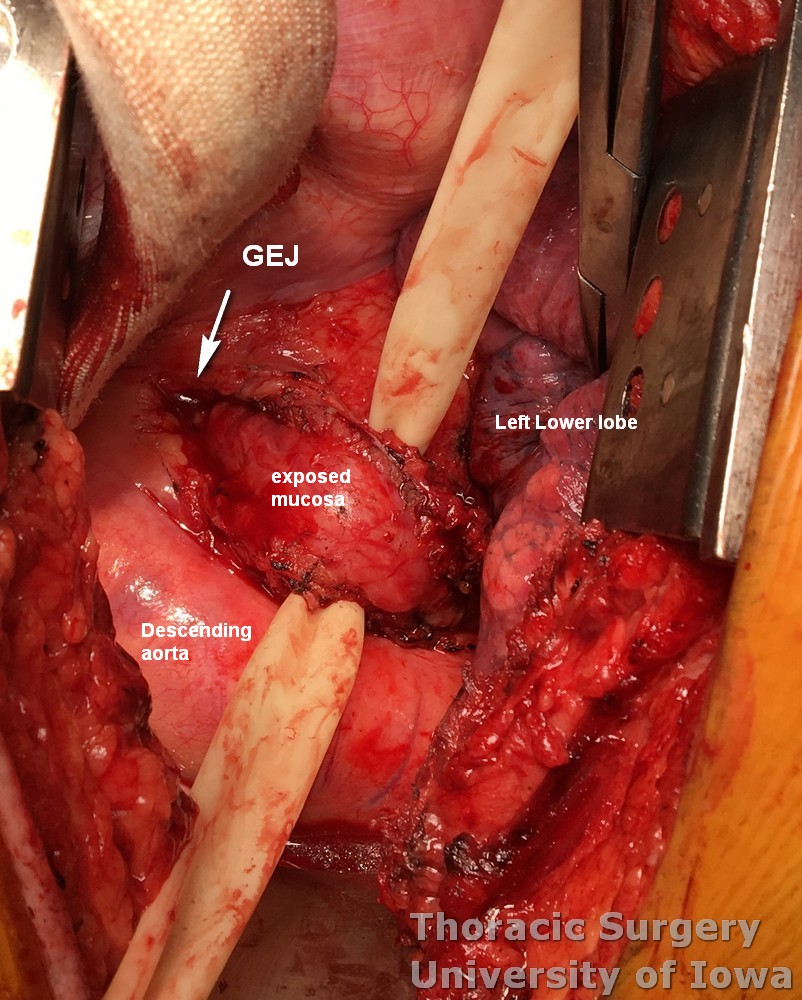
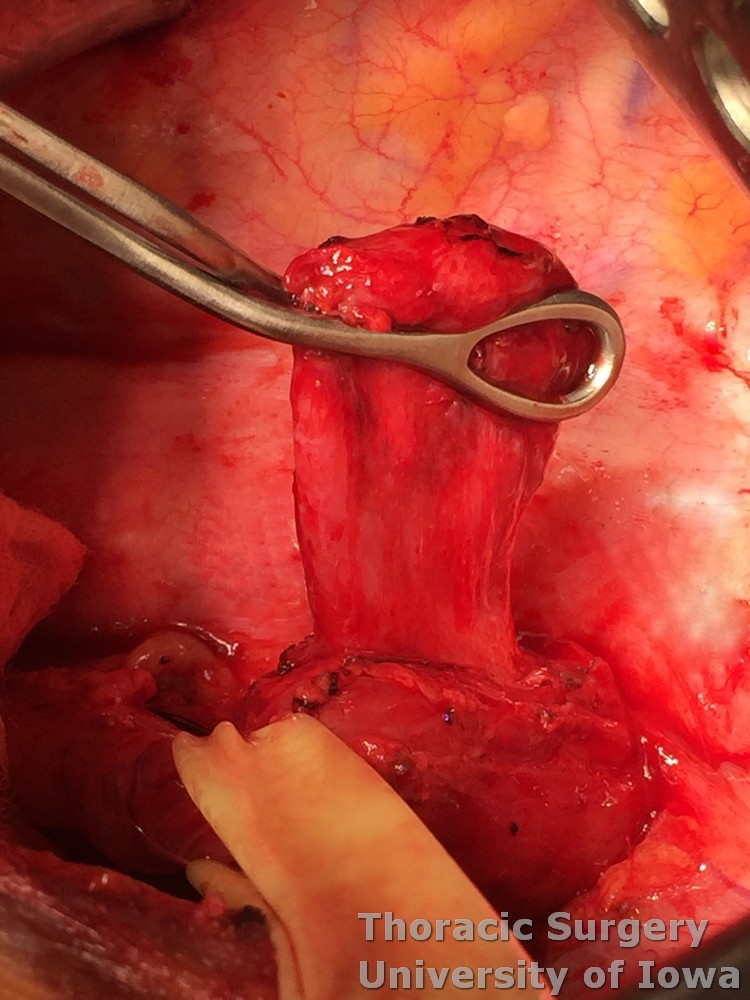
The diverticulum (D on the image below) is identified and the esophagus (E on the image below) is mobilized circumferentially and encircled with a Penrose drain to provide gentle traction.
-
Take care to identify and protect the vagus nerves.
-
Avoid excessive traction to the esophagus to prevent trauma.
-
Coexisting hiatal hernia (like on the image below) may be present
-
-
Free the esophagus between the inferior pulmonary vein and the diaphragm for improved mobility and exposure. The GEJ is delivered into the chest through the hiatus is myotomy is planned to be extended onto the stomach.
-
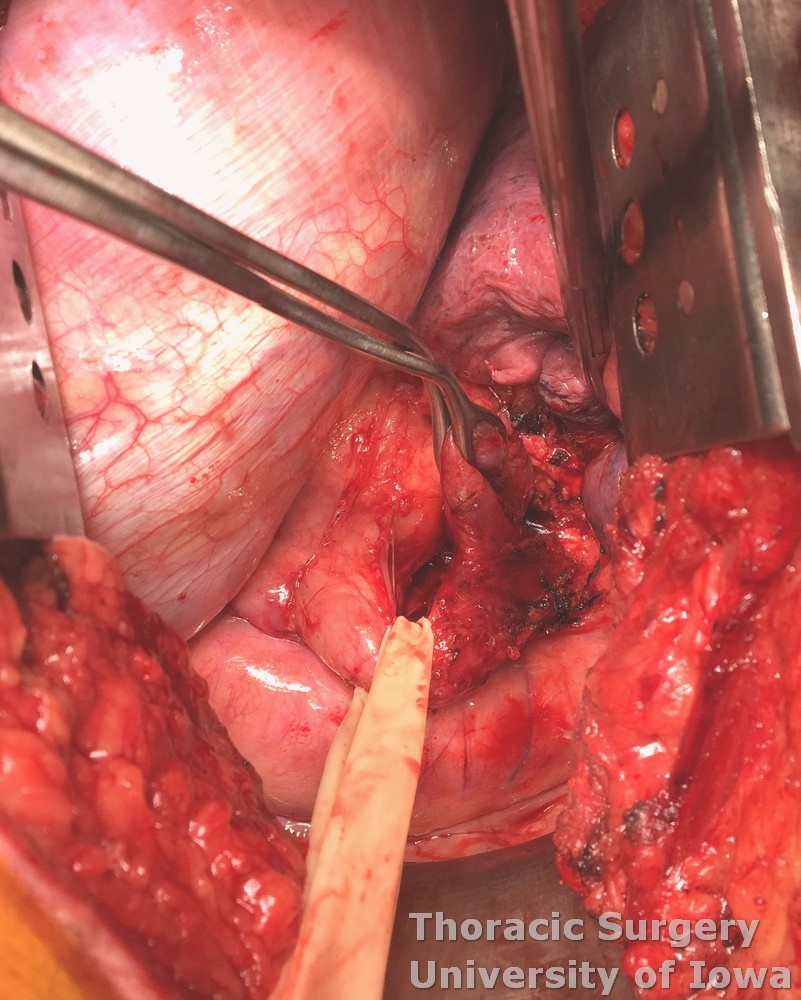
Most diverticula are directed towards the right chest and have adhesions to the mediastinum. Gently elevate the diverticulum with a ring clamp and dissect adhesions to expose its neck.
-
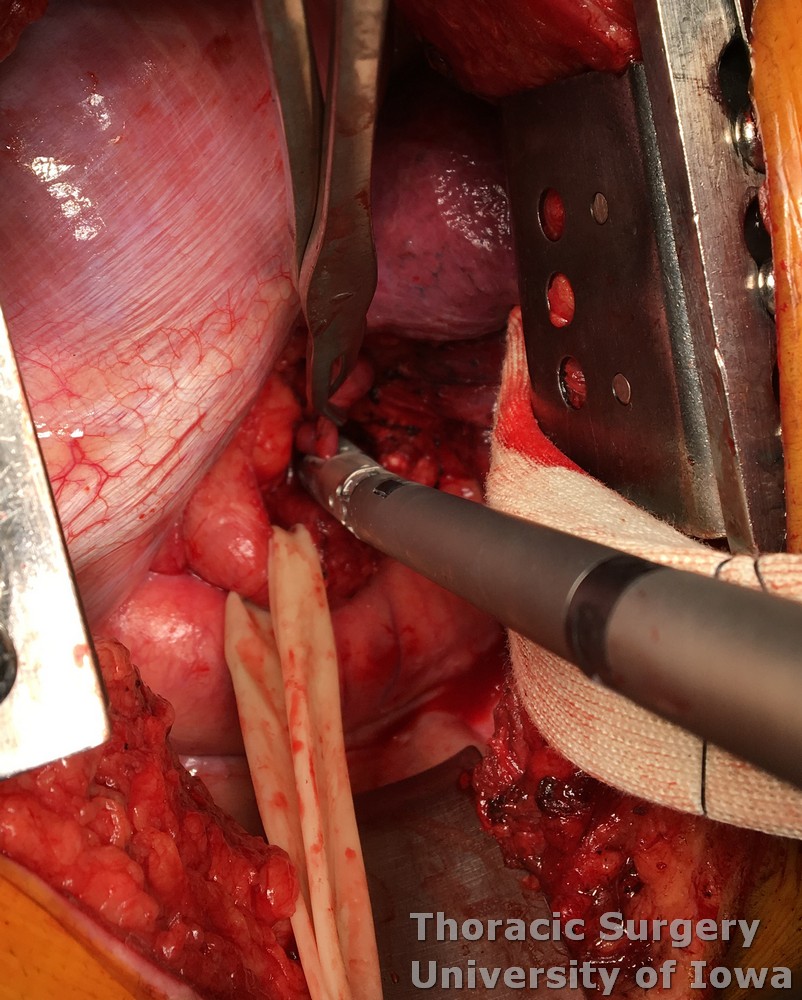
The EGD scope is removed and the anesthesiologist introduces a large, weighted bougie (56 Fr) transorally into the stomach. Surgeon-assisted guidance prevents bougie placement in the diverticulum.
-
Alternatively diverticulectomy and myotomy may be performed with gastroscope in the esophagus acting as a bougie to prevent narrowing of the lumen.
-
An endoscopic linear cutting stapler (blue or purple load depending oh hospital supplies) is positioned flush against the esophagus, and the diverticulum is resected. Alternatively diverticulum can be sharply excised and esophagus closed with the sutures.
-
Alternatively myotomy may be performed before diverticulectomy
-
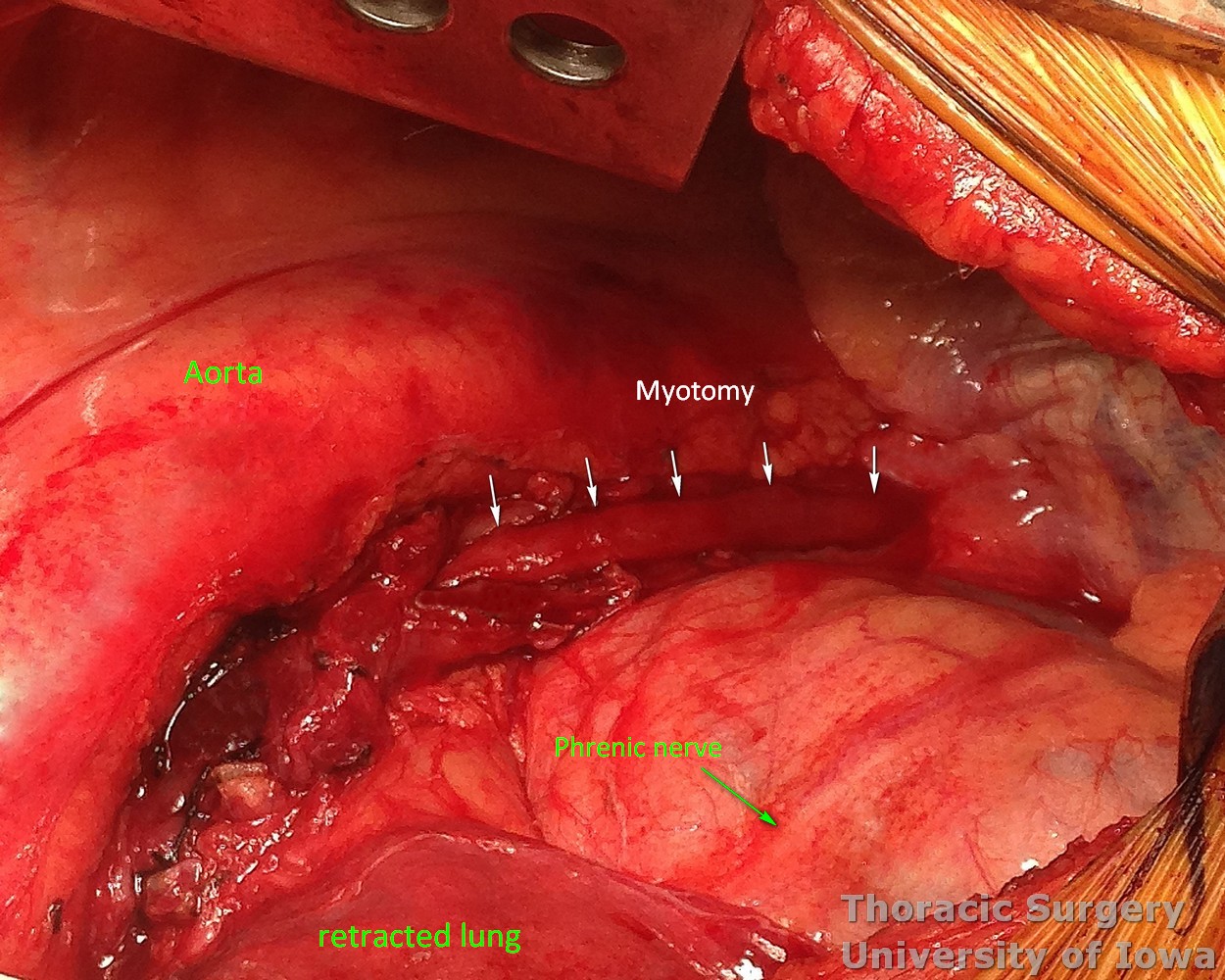
A wide esophageal myotomy is performed 90 degrees away from the diverticulectomy site. Use the right angle dissector to elevate the muscle layer and protect underlying mucosa.
-
The myotomy must be extended proximally above the level of the diverticulum or above the highest diverticulum if cases of multiple diverticula.
-
Distally the myotomy may on may not need to be extended across the GEJ on to the stomach depending on the preoperative manometry data.
-
For mid-esophageal diverticula, the myotomy ends up fairly long - frequently from the level of the aortic arch to the GEJ ( extent marked with arrows on the image below).
-
For epiphrenic diverticula, myotomy is not as long.
-
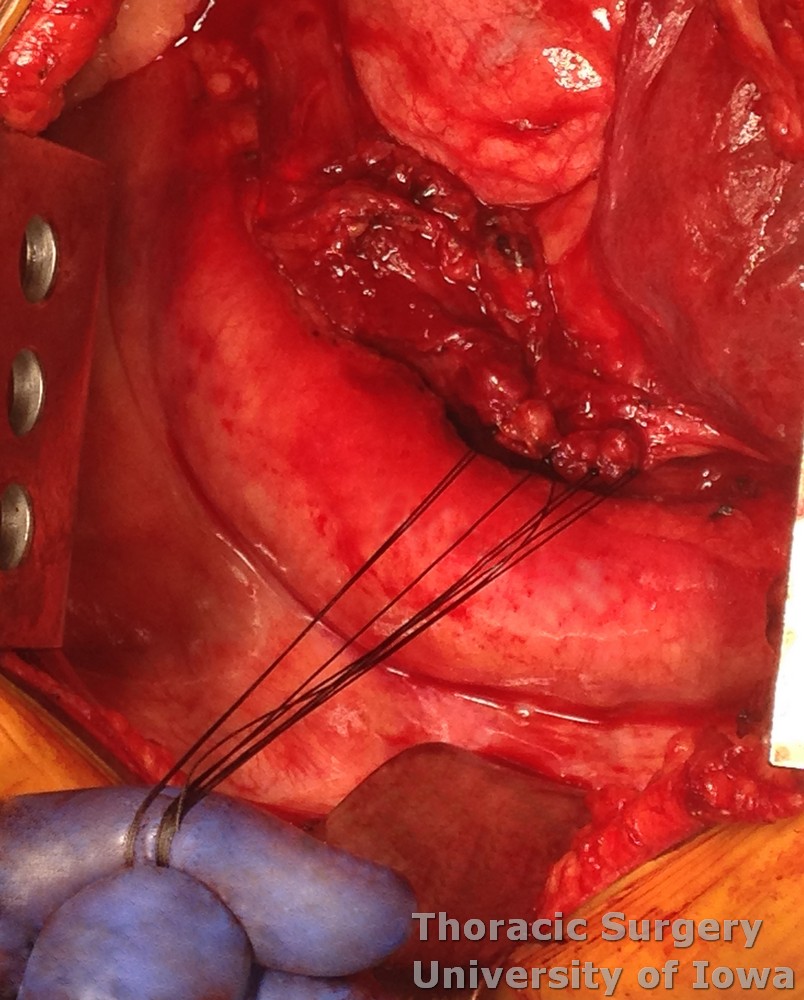
If myotomy is extended across the GEJ on to the stomach (2–3 cm for the hypertensive LES), consideration needs to be given for up to 50 % incidence of subsequent gastroesophageal reflux and concomitant antireflux procedure (partial fundoplication) may need to be performed.
-
The muscle is then closed over the diverticulectomy site with interrupted absorbable suture.
-
Submerge the esophageal staple line under normal saline. A surgeon will insufflate the esophagus with air under direct endoscopic vision. Observe for air leaks at this time.
-
On the endoscopic image note the diverticulectomy site (arrow) and prominent translumination distally at the myotomy site.
Completion of the thoracic phase
-
The EGD is withdrawn, and a 16–18 Fr nasogastric tube is guided into the stomach with surgeon assistance. NG is secured with a tape or magnetic bridle and placed on low- continuous suction (LCS).
-
One or two 28-32 Fr chest tubes are placed and secured to the skin with 0-monofilamanr suture.
-
The ribs are re-approximated with figure-of-eight pericostal #2 absorbable sutures.
-
The latissimus dorsi and serratus anterior fascia are re-approximated with running 0-absorbable suture.
-
The dermal layer and subcuticular layer are closed with running 2-0 and 4-0 absorbable suture, respectively. Surgical dressing or skin adhesive is used to cover incision.
POSTOPERATIVE CARE
General
-
The patient is extubated in the operating room and admitted to a general care surgical ward.
-
Pain control provided via epidural catheter limiting systemic narcotic analgesics.
-
CXR is obtained immediately postoperatively. Daily CXR are not needed unless a change was made in the chest tube management or patient’s condition changes.
-
Isotonic fluids are used to maintain euvolemic balance, with close attention to in-and-out (I/O) fluid measurements.
-
Perform urine output checks every 4 h. Consider removing indwelling urinary catheter after post-operative day 3 if patient is at low risk for having benign prostatic hyperplasia (BPH). Otherwise urinary catheter is kept while epidural is in place.
-
The head of bed is maintained at 45o to reduce the risk of aspiration.
-
NG tube to low (<80 mm Hg) continuous suction (LCS): Every 4 hours the drainage channel is flushed with 20 cc of fluid and the air channel is flushed with 20 cc of air to assure proper function of the NG tube. NG is removed after recovery of bowel function and esophagram demonstrating no leak.
-
Chest tube is maintained on suction at –20 cm H2O (off suction for ambulation) for first 1-2 days and then water sealed. Chest tube is removed after no air leak was observed for 24h, negative esophagram and its output is non chylous and <200 ml per day.
-
Aggressive pulmonary care.
-
Ambulation at least four times daily is recommended.
-
Incentive spirometer every our hour.
-
Vibrating Positive Expiratory Pressure therapy every our hour.
-
Scheduled bronchodilators every 4 hours
-
Scheduled chest physical therapy with the use of manual Pneumatic Percussor on both lung fields every 4 hours while awake. Manual percussion even of the operative side is well tolerated by patients and may be more effective than a built in percussion function of hospital beds.
-
Use mucolytics (Acetylcysteine ) inhalers as needed
-
-
Postoperative prophylactic antibiotics are not indicated.
-
Prophylactic heparin may be administered on POD 1
Specifics
-
PODs 1 and 2: pay attention to hemodynamics, fevers, in and out fluids, electrolytes, pulmonary care, pain control and ambulation.
-
Start home medications via NG tube that have no IV equivalent.
-
POD 2 or 3: Perform esophagram (start with water-soluble contrast followed by thin barium). If there is no esophageal leak then the NG tube may be removed, and a clear liquid diet may be started.
-
Discharge with instructions for clear liquid diet (total 3 days), followed by full liquid diet (total 3 days), followed by a soft-food diet until follow-up.
OUTPATIENT FOLLOW UP
-
Close phone follow-up by thoracic nurses.
-
Follow up in clinic in 2 weeks with CXR AP/PA.
-
Follow up in 1 year with esophagram.