Return to: Superior Laryngeal Nerve Blocks Instruction Video; Overcoming Gag Reflex for Awake Transnasal Laryngeal Surgery Case Example
Transoral injection laryngoplasty with videostroboscopy; Lingual Nerve Block (selective anesthesia for tongue and floor of mouth)
see also: Maximum Recommended Doses and Duration of Local Anesthetics
The glossopharyngeal nerve descends from the jugular foramen postero-medial to the styloid process along the posterior side of the stylopharyngeal muscle to branch at the level of the middle constrictor to provide sensory innervation to the posterior third of the tongue, the vallecula, the anterior surface of the epiglottis, the tonsils and pharyngeal wall (Faik 2002 and Pintaric 2016).
Administering anesthesia to the glossopharyngeal nerve (glossopharyngeal nerve block) has been described by and extraoral and two distinct approaches to intraoral.
Anterior Tonsillar Pillar Approach (intra-oral approach):
Click on Video Below:
a. Extraoral peristyloid approach (not recommended for temporary nerve blocks for anesthesia of the oropharynx)
- (used for treating glossopharyngeal neuralgia) as reported by Singh (Singh 2013)
- Introduce a needle percutaneously 3.5 - 4.5 cm deep, touch the styloid process and inject the drug behind it.
- Despite use of fluoroscopy - still considered difficult
- May be accompanied by concurrent block of the vagus nerve with associated hoarseness and difficulty swallowing
- Bilateral peristyloid GPN blocks considered a risk to develop bilateral vagal nerve paralysis
b. Intraoral Glossopharyngeal Nerve Block (GPN block) - each injection technique emphasizes aspiration before injection to avoid intravascular injection with additional potential for hematoma and ecchymosis
as per Pintaric (2016)
- Administer topical anesthesia to oropharynx
- 5 mL of local anesthetic using a 22- or 25- gauge spinal needle after the tongue is displaced int anteroinferior direction.
- Listed as potentially being associated with 'lasting oropharyngeal discomfort' (Sitzman 1997)
- Described as useful for neuralgia, abolishing gag reflex for surgery or endodontics, managing postoperative pain after tonsillectomy
as per Sitzman (1997) study of awake direct laryngoscopy - various approaches to glossopharyngeal nerve block - topical vs injection - concluded the gargle and 10% spray preferred to GPN block by injection
- Randomized single-blinded cross-over desing (N=11) volunterers subjected to all three approaches: gargle alone (2% visocus lidocaine); gargle and spray (10% lidocaine spray) and gargle followed bilateral GPN blocks
- swish and gargle 15 ml of 2% viscous lidocaine for two minutes then expectorate
- 10% oral Xylocaine spray 100 mgas single sprays bilateral to soft palate, posterior oropharygneal wall, palatopharyngea ach and BOT with two sprays to vallecula (10 sprays total)
- inject 1% lidocaine bilateral to block the GPN
- each received an IV with 0.2mg of glycopyrrolate as antisialoagogue 30 minutes before each procedure
- Procedure then performed 5 minutes after anesthesia: Macintosh-3 blade with sufficient force to sustain a grade 1 or 2 vies ofr 20 seconds
- "Anterior Tonsillar Pillar Method"
- 22 gauge Quincke spinal needle inserted to depth of 0.5 cm at base of atnerior tonsillar pillar (where BOT opposes the palatoglossal fold)
- After negative aspiration, 5 cc of 1% lidcoaine HCT plain slowly injected bilaterally
- Commented by authors: volume of 5 ml of local anesthetic used to produce a superior laryngeal nerve block as well (citing Stone DJ 1994)
- Oropharyngeal discomfort lasting 24 h or more was reported by 91% who received the block; discomfort lasting 3 or more days by 36%
- Also reported marked antisialagogue effect lasting 8 hours or more
as per Ramirez et al (Ramirez 2013) a clinical trial of 100 patients undergoing upper GI endoscopy randomly selected glossopharyngeal blocks with injection versus topical anesthesia concluded better with GPN blocks
- Glossopharyngeal nerve blocks provided greater comfort and reduced need for sedation compared to topical
- Glossopharyngeal nerve blocks
- IV midazolam 2-3 minutes before the glossopharyngeal nerve block
- 22 gauge needle 32 mm in length using total of 60 mg of lidocaine (2% solution) - 30 mg to each side
- retract tongue medially with needle inserted under the mucosa at the base of the pillar, 0.5 cm lateral to the base of the tongue.
- "Blockage was verified by gag reflex provocation after 3 minutes of latency, and then the endoscopic procedure began"
- Topical Anesthesia
- 30 mg of lidocaine spray administered in 3 consecutive 30 second intervals, each consisting of 10 sprays (10 mg/dose) of Xylocaine Pump Spray 10% (Astra Zeneca) and
- 2-3 minutes later, midazolam administered and titrated
"Posterior Tonsillar Pillar Method"
- local anesthetic injected near the base of the posterior tonsillar pillar
- requires wider mouth opening and displacement of tongue for access
"Anterior Tonsillar Pillar Method" as per Garg (Garg 2014 citing Benumof 1991) and Artime (Artime 2017)
- Tongue displaced medially (less of a gag) with easier exposure and better tolerated than Posterior Tonsillar Method (widely supported as 'better' by others including Henthorn (Henthorn 1995))
- Retraction forms a gutter or trough along floor of mouth between tongue and teeth
- The gutter ends in a cul-de-sac formed at the base of the anterior tonsillar pillar (palatoglossal arch)
- As per Artime (Artime 2017)
- 25 gauge spinal needle inserted 0.25 to 0.5 cm deep at the base fo the palatoglossal arch just lateral to the base of the tongue
- Aspirate (if air aspirated, have placed to far and withdraw back; don't inject if blood aspirated)
- 2 mL of 1% to 2% lidocain is injected (alternative of use of cotton-tiped swab soaked in 4% lidocaine)
References
Rao S, Rao S.Glossopharyngeal Nerve Block: The Premolar Approach.Craniomaxillofac Trauma Reconstr. 2018 Dec;11(4):331-332. doi: 10.1055/s-0037-1606249. Epub 2017 Aug 25.
Pintaric TS Upper Airway Blocks for Awake Difficult Airway Managmeent Acta Clin Croat 2016 Mar;55 Suppl 1:85-9
Faik OM, Ugur T, Memet OM, Necmett PM. Anatomic landmarks of the glossopharyngeal nerve: a microsurgical anatomic study. Neurosurgery. 2003;52(6):1400-10.
Singh PM, Dehran M, Mohan V, Trikha A, Kaur M. Analgesic efficacy and safety of medical therapy alone vs combined medical therapy and extraoral glossopharyngeal nerve block in glossopharyngeal neuralgia. Pain Med. 2013;14:93-102. doi: 10.1111/pme.12001.
Sitzman BT, Rich GF, Rockwell JJ, Leisure GS, Durieux ME, DiFazio CA. Local anesthetic administration for direct laryngoscopy. Are glossopharyngeal blocks superior? Anesthesiology. 1997;86(1):34-40.
(cited by Sitzman)- Stone DJ, Gal TJ: Airway management Anesthesia, 4th ed. Edited by Miller RD. New York, Churchill Livingstone, 1994, pp 1424-5
Garg R, Singhal A, Agrawal K, Agrawal N. Managing endodontic patients with severe gag reflex by glossopharyngeal nerve block technique.J Endod. 2014 Sep;40(9):1498-500. doi: 10.1016/j.joen.2014.01.028. Epub 2014 Mar 6
(cited by Garg) Benumof JL. Management of the difficult adult airway. Anesthesiology 1991;75: 1094–6.
Barton S, Williams JD. Glossopharyngeal nerve block. Arch Otolaryngol 1971;93: 186–7.
Steven D. Waldman MD, JD Glossopharyngeal Nerve Block: Intraoral Approach [Book Chapter] in Atlas of Interventional Pain Management, Chapter 25, 91-94.e1
Artime C and Sanchez A: Preparation of the Patient for Awake Intubation. [Book Chapter] in Hagberg and Benumof's Airway Management, 12, 216-234.34 4th edition 2017
Hannallah M and ElDAbh A: Glossopharyngeal nerve bklock for esophagogastroduodenoscoopy in critically ill patients. Anaesthesia, Pain & Intensive Care. ISSN 1607-8322, ISSN (Online) 2220-5799
Henthorn R, Ahmed A, and Raghuvender G: Which Method for Intraoral Glossopharyngeal Nerve Block is Better? Anesthesia & Anagesia: November 1995 - Volume 81 - Issue 5 - p 1113-1114 Letter to the Editor
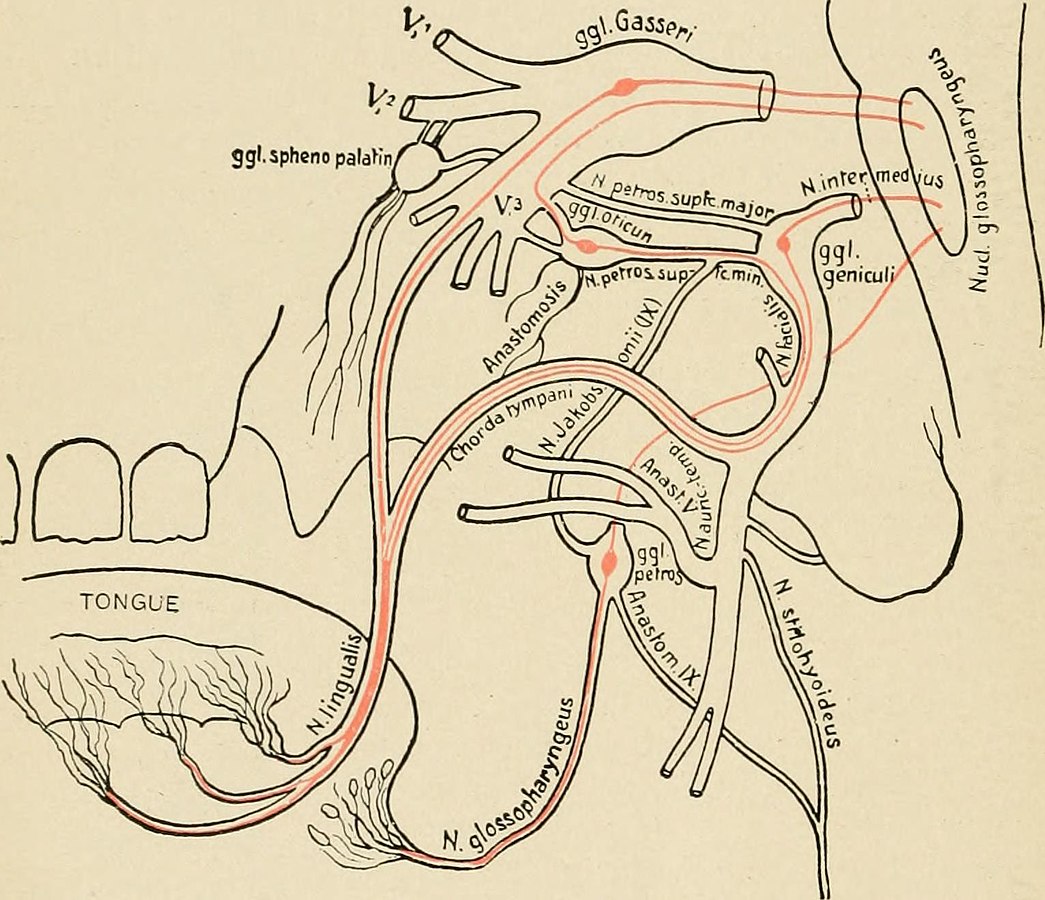
With permission from wikicommons - By Internet Archive Book Images - https://www.flickr.com/photos/internetarchivebookimages/14767286011/Source book page: https://archive.org/stream/textbookofhumanp00tige/textbookofhumanp00tige..., No restrictions, https://commons.wikimedia.org/w/index.php?curid=43366675
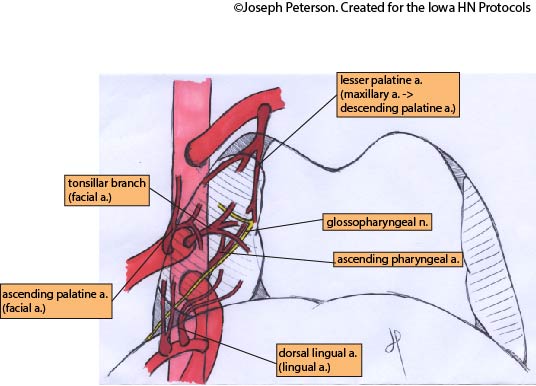
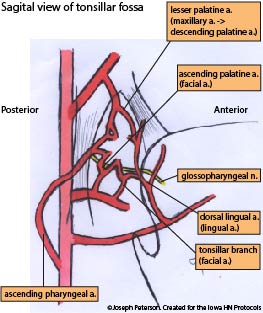
with permission from wikicommons By Anatomist90 - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=23581018
