click on image to enlarge; advance with cursor over border
return to: Salivary Gland Surgery Protocols
see also (video): Shaw Hemostatic Scalp for Parotidectomy
Case examples:
Sialosis or sialadenosis Case example of surgical treatment
Case Example Parotidectomy with sacrifice of buccal branch (includes video demonstrating drain on postop day 1)
Parotidectomy: case example - multiple Warthin's tumors
Case Example Deep Lobe Parotid Tumor Parapharyngeal Space
see also: Preservation of branch of Great Auricular Nerve
Warthins tumor 'shell out' with facial nerve monitoring
Case Example Resection of Parotid Wharthins Tumor without Facial Nerve Dissection
Case Example Parotid Lipoma-like Liposarcoma
also: photos at bottom of page
GENERAL CONSIDERATIONS
-
Indications
-
Parotid neoplasm: The presence of an unexplained mass in the parotid gland warrants consideration for parotidectomy to be done both for diagnosis and treatment. In our hands it is rare to do a parotidectomy for tumor without first doing a needle biopsy.
-
Chronic parotitis refractory to medical management or management with sialendoscopy
-
Sialendoscopy with duct dilation, stone removal, or steroid/antibiotic insufflation extends the number of options for surgical treatment beyond parotidectomy
-
Parotidectomy may be required as a treatment either for unsuccessful sialendoscopy or as management of complication following sialendoscopy
-
-
To ensure adequate deep margins for resection of cheek skin malignancy (see Melanoma (Evaluation and Management) (8th Edition AJCC) protocol)
-
Resection of lymph nodes either identied as harboring metastases or at risk for metastases. A melanoma on the cheek with a positive sentinel node in level I would warrant removal of intervening lymph nodes via parotidectomy in the course of performing a neck dissection. A squamous cell carcinoma arising in the pre-auricular region with documented metastasis to level I would warrant an intervening parotidectomy.
-
-
Contraindications
-
Comorbidity precluding tolerance of general anesthesia
-
-
Parotid lesions
-
Specific Benign Lesions
-
Pleomorphic adenoma common (see: Pleomorphic Adenoma; Pleomorphic Adenoma Radiology)
-
Recurrent Pleomorphic Adenoma (RPA)
-
Redaelli de Zinis 2008
-
33 patients with RPA
-
30.3% a branch of the facial nerve or the trunk was deliberately sacrificed
-
Multinodular lesion and type of intervention performed were significantly associated with higher probability of recurrence.
-
Frey syndrome occurred in 43% of patients
-
-
Makeieff 2010
-
Average years to recurrence = 11.4 years
-
Surgeons used facial nerve monitoring
-
A FN branch had to be resected in 11.2% of cases
-
Carcinoma ex-Pleomorphic Adenoma in 16.1% of cases
-
FN palsy at 1 year (House-Brackmann >or = 3) was 11.3%
-
62.9% of pleomorphic adenomas were multinodular on pathology and only 44% were multinodular on MRI (indicator of high rate of recurrence)
-
-
-
Warthin's
-
Lipoma: rare (0.5-4% of all parotid masses). Difficult to distinguish from Liposarcoma preoperatively. Most advocate facial nerve dissection for removal; low rate of recurrence
-
-
Malignant
-
Mucoepidermoid carcinoma
-
Adenoid cystic carcinoma
-
Metastases to parotid
-
-
-
See: Parotid neoplasm management
-
Pertinent anatomy
-
The Parotid gland is a serous secreting gland, and the largest of the major salivary glands. It is located posterior and lateral to the mandibular ramus and anterior to the SCM. The posterior belly of the digastric and stylohyoid muscles lie deep to the gland. The gland is innervated by postganglionic parasympathetic fibers from the otic ganglion via the auriculotemporal nerve. The parotid duct extends from the anterior border of the gland, travels over the masseter muscle to penetrate the buccinator muscle and open into the oral cavity, adjacent to the second upper molar ipsilaterally.
-
It is common to see accessory parotid glands distally along the parotid duct, and these are termed socia parotidis.
-
The retromandibular vein is used as a landmark when evaluating imaging studies, as this vein marks the division of the deep and superficial lobes. This relationship is important as it approximates the depth of the facial nerve.
-
This gland is encased in parotid fascia (superficial layer of the deep cervical fascia).
-
PREOPERATIVE PREPARATION
-
Evaluation
-
Fine needle aspiration in the majority of cases - best done with ultrasound guidance for the great majority of cases (see specific examples of Salivary Gland Pathology on the Head and Neck Pathology page)
-
MRI if consideration for deep lobe/parapharyngeal space/perineural spread
-
CT if concern for adjacent bone invasion
-
-
Consent
-
Describe procedure, incision, facial nerve dissection
-
Recent study by Lydiatt, on litigation for facial nerve paralysis, detailed the importance of informed consent as well as detailed explanation of risks including but not limited to facial paralysis and paresis.
-
Consideration for more aggressive behaving masses: mandibulectomy, temporal bone resection. If there is a suspicion that the facial nerve may need to be sacrificed, be prepared for primary nerve or cable graft repair with great auricular, sural, or accessory nerve (if removed in neck dissection).
-
Describe potential for neck dissection if final specimen at time of surgery shows intermediate or high-grade malignancy. Neck dissection may range in scope from removal of upper Level I and II nodes (as accessed through Blair incision) to possible radical neck dissection (if metastatic disease seen at time of surgery).
-
Describe expected sequelae
-
Numb about incision and ear
-
Soft tissue depression from removal of parotid and tumor
-
Facial nerve weakness, usually temporary (Rate of paresis and paralysis, respectively after parotidectomy: 1) partial- 1.9%/0.7%; 2) superficial- 22%/2%; 3) Total 46%/10%)
-
-
Describe potential complication
-
Bleeding, infection, reaction to anesthesia
-
Specific: salivary fistula, permanent facial nerve injury
-
Frey's Syndrome (gustatory sweating)
-
First bite syndrome - thought to be caused by sympathetic denervation of the parotid
-
-
NURSING CONSIDERATIONS
-
Room Setup
-
Instrumentation and Equipment
-
-
Special
-
Jackson-Pratt bulb suction drain
-
Shaw scalpel
-
Nerve stimulator control unit and instrument (Parsons McCabe)
-
Nerve integrity monitoring system (NIMS)
-
-
-
Medications (specific to nursing)
-
Antibiotic ointment
-
1:100,000 epinephrine injection (no lidocaine) for skin incision
-
-
Prep and Drape
-
Standard prep, 10% povidone iodine, 5% povidone iodine periorbital areas
-
Drape
-
Head drape
-
Place towels so the ear, mastoid tip, and sternocleidomastoid (SCM) muscle are well exposed, with a towel placed from midline forehead to mentum to expose ipsilateral half of the face
-
Place steridrape over face to allow inspection of the corner of mouth and eye through the drape
-
Split sheet
-
-
-
Drains and Dressings
-
400 cc bulb suction drain with 10 mm fully perforated Jackson-Pratt drain
-
Pressure dressing is used with a Penrose drain, including fluffs and burn netting around neck
-
Adaptic, large, 3 x 8 inch
-
Fluffs, sterile, 5-pack x 2
-
Kling, 4 inch
-
-
Special Considerations
-
Nerve integrity monitoring system has become more routine and is most useful for recurrent tumors or difficult dissections.
-
All muscle relaxants should be reversed before prepping and draping.
-
Do not use lidocaine; it may anesthetize the nerve.
-
Shaw hemostatic scalpel and controller are available (place in metal basin with wet towel for fire prevention).
-
ANESTHETIC CONSIDERATIONS
-
Induction
-
Antibiotics begun with placement of the IV (see Antibiotic Prophylaxis in Head and Neck Surgery protocol). Although the case is usually clean, the interruption and retention of salivary tissue may create an environment for bacterial sialadenitis to develop. If there is a component of chronic sialadenitis, my consider leaving patients on antibiotics for 5 to 7 days (converted to oral antibiotics once feeding is begun).
-
Although not necessary for all cases, nasotracheal intubation through the nostril contralateral to the tumor may occasionally be preferred in selected cases. Maintenance of the airway by this method permits complete closure of mouth with approximation of the teeth potentially (not usually an issue) allowing better access to deep lobe tumors that have parapharyngeal extension.
-
Do not paralyze patient (we may employ a facial nerve stimulator).
-
-
Positioning
-
Table turned 180° (head away from anesthesiologist) for cases requiring involved dissection (notify anesthesia preoperatively of need for extra long tubing). May turn just past 90° for tail of parotid lesions and simple dissections.
-
Head of bed is elevated to diminish bleeding.
-
OPERATIVE PROCEDURE (operative note template)
-
Incision and Flap Elevation
-
Shaw electrical scalpel
-
120°F for skin
-
220°F for deeper tissue
-
270°F to coagulate bleeders
-
-
Doubly-modified Blair incision
-
Preauricular (above level of zygomatic arch)
-
Posterior extension to mastoid to enable full mobilization of tail of parotid
-
Inferomedial extension toward hyoid in neck skin crease
-
-
Flap elevation in similar plane to facelift ("cobble-stoning" of fat on undersurface of flap). Flap elevation may be safely performed at a slightly deeper plane – just superior to periparotid fascia – to diminish risk of symptomatic Frey's syndrome by making a thicker skin flap.
-
Posterior branches of the great auricular nerve may be preserved in the majority of cases in which case the lower part of the Blair incision is made over the SCM to identify the great auricular nerve before it branches. The incision of the skin about the ear lobe may injure the small superficial branches of the great auricular nerve. To avoid injuring these branches, the skin incision about the lobe is deepened in the course of dissecting the gr. auricular nerve branches superiorly. see: click on Preservation of branch of Great Auricular Nerve
-
-
Mobilization of Parotid in Preparation for VIIth Nerve Dissection
-
Elevate parotid tissue forward off SCM muscle with attempts to preserve posterior branch of great auricular nerve innervating lower external ear.
-
Place 2-0 silk "stay sutures" into ear lobe (subcutaneous) for posterior retraction and stay sutures into the cheek flap for anterior retraction and secure with Allis clamps to drapes (using hemostats ruins the hemostats).
-
Detach parotid from tragal cartilage with gentle anterior retraction on parotid with Allis clamps applied to periparotid fascia (and/or Sewell retractors).
-
Detach parotid from anterior SCM
-
Identify the digastric muscle and follow the lateral surface towards the mastoid tip.
-
Identify the facial nerve after obtaining this wide exposure employing landmarks.
-
Tympanomastoid suture by palpation (the most consistent landmark) (approximately 2mm inferior to suture)
-
Digastric muscle (nerve is immediately superior to digastric)
-
Tragal pointer: The facial nerve trunk is commonly found 1 cm inferior and 1 cm deep to the tragal pointer. This relationship may be altered by the presence of tumor, previous surgery, or infection.
-
The parotid-mastoid fascia is incised as the final step before identifying the trunk of the facial nerve. The nerve is found within fat deep to the parotid-mastoid fascia and localized employing the landmarks noted above.
-
The facial nerve stimulator may help to localize the nerve through stimulation with observation of facial movement
-
-
Other less common methods of facial nerve identification may be employed and should be chosen based on the disease present.
-
Approach main trunk retrograde through one of the branches of the facial nerve that may be found at predictable sites and confirmed with nerve stimulator.
-
Buccal branch: runs parallel to and 1 cm below the arch of the zygoma traveling toward the corner of the mouth. Thin-walled parotid duct travels closely adjacent, usually just below this branch. Care must be taken in retrograde dissection to ensure that adjacent branches in a more superficial plane are not injured.
-
Identify one of three eye branches where they cross the arch of the zygoma near the upper anterior corner of the gland.
-
Follow retromandibular vein superiorly noting that the branches of the cervicofacial division cross over it in intimate association in the majority (not all) cases - see discussion about variability of retromandibular vein and (Mahore 2018)
-
Partial removal of the mastoid process is done by chisel, rongeur, or drill to identify nerve in mastoid
-
Mandibular branch: identified as it creases the deep surface of the tail of the parotid with blunt freeing of the tail. This branch is also reliably found at the angle of the mandible. This approach is my (HH) preferred approach when a retrograde dissection is need.
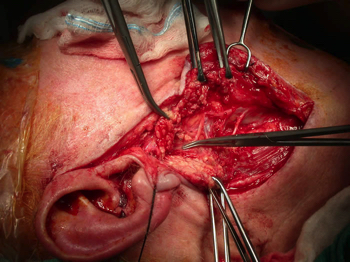
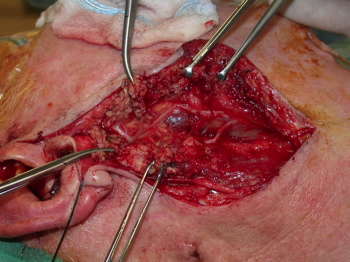
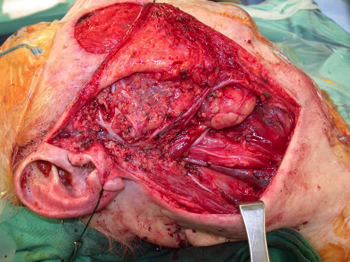
In the example below, a gamma probe is used to identify a sentinel lymph node (Tc 99 injection done several hours before). The sentinel node was overlying the lower division of the facial nerve, warranting identification and preservation of the nerve through retrograde dissection.
One week after the above dissection, the patient was returned to the O.R. for completion parotidectomy and neck dissection after pathology identified two sentinel nodes - each harboring 0.2 cm metastases (melanoma). The completion parotidectomy was done with retrograde dissection of the facial nerve (following the previously identified lower division) back to the main trunk followed by antegrade dissection with follow-up several months later after irradiation.
-
-
-
- Facial Nerve Dissection
- Initial course of nerve progresses from deep to superficial. A small right angle hemostat (or McCabe facial nerve dissector) is helpful for initial dissection, especially in obese patients.
- Careful blunt dissection immediately on epineurium of nerve with slow advancement and spreading action.
- Parotid tissue transected between tines of hemostat with Shaw scalpel (220°F) slowly and patiently to minimize bleeding. Alternatively, the Concept bipolar cautery or Harmonic scalpel may be used to divide parotid tissue to minimize blood loss.
- Identify pes anserinus. The pes anserinus is the main bifurcation of the facial nerve into the upper (temporofacial) and lower (cervicofacial) branches. The facial nerve further divides into 5 branches (the first 3 from the temporofacial division): temporal, zygomatic, buccal, marginal mandibular and cervical.
- The course of further dissection depends on location of tumor mass. It may be helpful to place large hemoclip in periparotid fascia overlying mass as a landmark to its location to help in avoiding dissection into tumor mass with tumor spill.
- Removal of a cuff of parotid tissue around tumor (without total lobectomy) is generally all that is necessary for benign tumors. Note that for many tumors, adequate resection will require excision of a portion of the underlying deep lobe. It is more logical to carefully attend to adequately addressing this deep margin than to routinely perform a comprehensive lateral lobe removal. The entire removal of the superficial parotid tissue may resect normal tissue many centimeters away from the tumor and leave close margins adjacent to the deep lobe remnant. Note that en bloc resection of a tumor with a cuff of surrounding normal tissue is usually possible only for tail of parotid lesions due to the constraints of facial nerve preservation.
- Initial course of nerve progresses from deep to superficial. A small right angle hemostat (or McCabe facial nerve dissector) is helpful for initial dissection, especially in obese patients.
- Completion of Procedure
- Accuracy in frozen section analysis of the parotid tumor is dependent on experience of pathologists. The "time honored" method has been to await permanent section report before sacrificing facial nerve, then return to operating room to complete resection following permanent histologic section analysis. Our method: review frozen section slides with pathologist. Facial nerve (or branch thereof) sacrificed only in case of malignancy or multiple recurrent pleomorphic adenomas. High-grade malignancy on frozen section assessment indicates need for more thorough, total or near total parotidectomy with upper-level neck dissection.
- General principle: If the facial nerve is working before surgery, every effort should be made to enable it to work after surgery, even if microscopic positive tumor margins are left on the nerve.
- Hemostasis performed with bipolar cautery.
- Irrigate copiously
- #10 fully perforated flat Jackson-Pratt drain is placed through stab incision in neck, away from direct contact with VII nerve. Use of closed suction for several days may decrease risk of seroma developing or salivary-cutaneous fistula.
- Skin closure is done with 3-0 or 4-0 vicryl or chromic subcutaneous and combination of running and interrupted 5-0 nylon to skin of the neck and 6-0 nylon to the face.
- Pressure dressing is used until patient is awake, then removed if suction drain is used. A tighter mastoid-like dressing with wrap-around neck is used in conjunction with a Penrose drain.
POSTOPERATIVE CARE
- The wound is exposed by removal of the pressure dressing after full emergence from anesthesia, usually on the ward later in the day (pressure dressings off).
- Suction drain management
- The suction drain is left in for 36 hours minimum (longer depending on output).
- General rule: Remove drain only after three consecutive 8-hour shifts demonstrate less than 30 cc total output.
- The drain may be managed in an outpatient setting. Secure the drain by placing 2-inch cloth tape to the shoulder and taping the tubing to the cloth with 2 inch clear tape. After demonstrating proficiency with caring for the drain, the patient may be discharged on postoperative day #1 with a scheduled return appointment on postoperative day #6 for suture and drain removal.
- Frey's syndrome
- Important to counsel patient in preoperative setting.
- Diagnosis is made by Minor's starch-iodine test. The ipsilateral face is painted with iodine and allowed to dry. Starch powder is dusted onto the face and the patient is given a sialogogue (lemon slice or drop). Dark blue staining reveals the area of gustatory sweating.
- Conservative treatment includes antiperspirants or topical 1% glycopyrrolate lotion. Injections of Botulinum toxin A to the affected area is also effective.
SAMPLE DICTATION
see also sample dictation for retrograde dissection of facial nerve and deep lobe (parapharyngeal space) tumor removal
-
The sample dictation below is not intended to be used as a template. It reflects only one of a multitude a variations on this procedure and should not under any circumstance substitute for the surgeon's own dictation. It is provided to help visualize the procedure from beginning to end and to illustrate key points.
Specify size of the lesion, location relative to the gland, whether the mass was removed in toto (whether the margins were grossly negative). If a frozen section was performed, a preliminary pathologic diagnosis should also be included. Specify if the facial nerve was spared, sacrificed or inadvertently transected. If the nerve was spared, document whether the nerve was stimulated before closure and whether stimulation produced the expected contraction of facial muscles.
Findings:
2 cm mass involving the right parotid gland in the mid portion of the parotid. The mass was completely removed with a cuff of normal-appearing parotid tissue. Frozen section were consistent with a pleomorphic adenoma. The facial nerve branches were spared and stimulation of the main trunk at the end of the procedure produced contraction of all facial muscles.
Description of Procedure:
Informed consent was reviewed with the patient in the preoperative evaluation area. The patient was brought to the operating room and placed on the operating table in the supine position. The patient was transorally intubated and the bed rotated 180 degrees (head away from anesthesia). A modified Blair incision was marked starting at a right pre-auricular crease and coursing behind the right ear lobule into a skin crease two fingerbreadths behind the angle of mandible. 10ml of epinephrine 1:100,000 was infiltrated along the planned incision line. The whole right side of the face prepped with Betadine and draped in sterile fashion with the right side of the face exposed through a sterile drape. A 15 blade was used to make the modified Blair incision, which was carried down to the level of the sternocleidomastoid muscle in the neck and the tragal cartilage anterior to the auricle. The great auricular nerve was identified with the posterior branches preserved and the nerve mobilized posteriorly out of the region of dissection. The posterior belly of digastric muscle was identified. The tragal cartilage pointer was identified. The intervening tissue spanning the two landmarks were carefully dissected until the facial nerve was identified in its usual location. Next, the skin flap was dissected off the parotid fascia until the leading edge was anterior to the parotid mass. The facial nerve was was then dissected out to the pes anserinus where the inferior and superior divisions were identified. The mass was identified between the inferior and superior divisions. The facial nerve branches around the tumor were dissected out past the mass so that the tumor could be peeled away from the facial nerve. In this fashion the mass was completely removed along with a cuff of normal-appearing parotid tissue on all sides with grossly negative margins. The mass was then oriented and sent to pathology. Frozen sections were obtained and indicated pleomorphic adenoma. The main trunk of the facial nerve was stimulated and caused contraction of all facial muscles supplied by the nerve. Bleeding was stopped with bipolar cautery and the wound was irrigated with sterile saline. A fully perforated soft-flat Jackson Pratt drain was then placed in the surgical bed and the wound closed in layers using 3-0 Vicryl sutures to reapproximate subcutaneous tissue and and running 5-0 nylon stitches to reapproximate the skin. The patient tolerated the procedure well, was extubated in the operating room and transferred uneventfully to the post anesthesia care unit. (see drain management protocol: Closed Suction (Jackson Pratt) Drain Placement and Removal; Closed Suction Drain Management - Securing the Drain; Closed Suction Drain Management)
SUGGESTED READING
Conley J. Search for and identification of the facial nerve. Laryngoscope. 1978;88:172-175.
Graham SM, Hoffman HT. Extra-temporal facial nerve injury: avoidance and pitfalls. Submitted to Otolaryngol Head Neck Surg.
Hoffman H, Funk G, Endres, G. Evaluation and surgical treatment of tumors of the salivary glands. In: Themley SE, Ponje WR, Botskis JG, Lindberg RD, eds. Comprehensive Management of Head and Neck Tumors. 2nd ed. Philadelphia, PA: WB Saunders; 1999.
Hoffman HT, Karnell LH, Pinkston R, Robinson RA, Menck HR. The national cancer data base report on cancer of the head and neck: acinic cell carcinoma. Head Neck. 1999;21:297-309.
Lam KH, Wei W, Ho HC, Ho CM. Whole organ sectioning of mixed parotid tumors. Am J Surg. 1990;160:377-381.
McCabe BF, Work WP. Parotidectomy with special reference to the facial nerve. Otolaryngology. 1968:IV(Sec III):37-53.
Lydiatt, DD. Medical Malpractice and Facial Paralysis. Arch Otolaryngol Head Neck Surg. 2003;129:50-53.
Stennert E, Wittekindt C, Klussman PJ, Arnold G, Guntinas-Lichius O. Recurrent Pleomorphic Adenoma of the Parotid Gland: A Prospective Histopathological and Immunohistochemical Study. The Laryngoscoe. 2004;114:158-163.
Harell, M, Levy, D, Elam, M. Superficial parotidectomy for benign parotid lesions. Operative Techniques of Otolaryngology, Dec. 1996 Vol 7 (4); 315-322.
Redaelli de Zinis LO, Piccioni M, Antonelli AR, Nicolai P. Management and prognostic factors of recurrent pleomorphic adenoma of the parotid gland: personal experience and review of the literature. Eur Arch Otorhinolaryngol. 2008 Apr;265(4):447-52.
Makeieff, M, Pelliccia P, Letois F, Mercier G, Arnaud S, César C, Garrel R, Crampette L, Guerrier B. Recurrent Pleomorphic Adenoma: Results of Surgical Treatment. Ann Surg Oncol. 2010 Jul 20.
Witt RL, Weinstein GS, Rejto LK. Tympanomastoid suture and digastric muscle in cadaver and live parotidectomy. Laryngoscope. 2005 Apr;115(4):574-7.
Note the variability in anatomic relationships between the retromandibular vein and facial nerve. As per Mahore et al (Mahore 2018), the retromandibular vein has been reported as passing lateral to the facial artery in 12.5% of cases with other anatomic studies identifying the retromandibular vein lateral to the facial artery in 17% (Kim 2009), 28% (Toure 2010), and 10% (Kopuz 1995). In rare cases the facial nerve may be encircled by a venous ring formed by the retromandibular vein.
Mahore D, Mangalgiri AS, Namdev LN, Kapre M.Variations of Retromandibular Vein and Its Relation to Facial Nerve Within Parotid Gland. Indian J Otolaryngol Head Neck Surg. 2018 Sep;70(3):395-397. doi: 10.1007/s12070-018-1389-1. Epub 2018 May 8.
Kim DI, Nam SH, Nam YS, Lee KS, Chung RH, Han SH The marginal mandibular branch of the facial nerve in Koreans. Clin Anat 22:207–214 (2009)
Toure´ G, Vacher C (2010) Relations of the facial nerve with the retromandibular vein: anatomic study of 132 parotid glands. Surg Radiol Anat 32:957–961
Kopuz C, Ilgi S, Yavuz S, Onderog˘lu S (1995) Morphology of the retromandibular vein in relation to the facial nerve in the parotid gland. Acta Anat 152(1):66–68




