return to: Total Laryngectomy; Laryngeal Surgery (Malignant Disease) Protocols; Case Example Tracheoesophageal puncture with Cigla Percutaneous Trach set Atos TEP inserter
see also: Esophageal Speech without TEP compared to with TEP
return to: Botulinum Toxin Protocols
(Under Local Anesthesia and Under General Anesthesia)
GENERAL CONSIDERATIONS
Voice production after total laryngectomy may be effected by mechanical means through an electrolarynx or vibration as air passes through the pharyngoesophageal (PE) segment. Esophageal speech, which is dependent on regurgitation of air accumulated in the esophagus and stomach, offers the significant advantages of independence from prosthetic devices and voice production without the need for digital occlusion of the tracheostoma. Speech through voice production created by passage of air through a valve positioned in the party wall between the trachea and pharynx or upper esophagus (tracheoesophageal puncture [TEP] speech) is dependent on a prosthesis. TEP speech can be effected without digital occlusion of the tracheostoma by use of a housing glued over the tracheostoma permitting inspiration of air with a portion of the expired air redirected through the TEP prosthesis. TEP speech is lung powered speech and, as such, may offer more durable and louder speech than esophageal speech.
Click here to view video of updated use of Ciaglia perc trach set with Atos Medical TEP inserter:
video
TEP Cigla
Click here to view a Tracheoesophageal Puncture (TEP) Technique with Initial Voice Training employing Ciaglia Blue Rhino percutaneous tracheotomy technique with initial clinic visit 6 days later with initial voicing techniques employing In-Health Manometer.
Click here to view a another video of a TEP employing Ciaglia Blue Rhino percutaneous tracheotomy technique with results two week later.
PREOPERATIVE PREPARATION
- During Examination, Ensure Adequate
- Stoma size
- Manual dexterity
- Pulmonary reserve
- Preoperative Speech Therapy Consultation (to help in assessing suitability for TEP)
- It is helpful to discuss with the Speech Pathologist that the patient will be working with as to the size of red rubber catheter to insert to fit the planned prosthetic.
- Preparation (for procedure done under local anesthesia)
LOCAL ANESTHESIA
This approach was done commonly in the clinic (surgicenter) but had drawbacks to it - leading to our more common management under general anesthesia with (usually) immediate placement of prosthesis as shown in the video. The care of a new TEP after placement of the red rubber catheter is available at: staged approach Tracheoesophageal_Fistula.pdf
NURSING CONSIDERATIONS (Local Anesthesia)
- Room Setup
- Basic Soft Tissue Room Setup
- Done in the Surgicenter in the Otolaryngology Clinic
- Instrumentation and Equipment
- Standard
- Bipolar Forceps Trays
- Minor Instrument Tray, Otolaryngology
- Maloney Esophageal Bougie Instrument Tray (older dilators contained
- mercury and had to be emptied of it; those in current use do not
- contain mercury)
- Special
- Red rubber catheters: 12, 14, and 16 Fr. (good to confer with speech pathology pre-treatment to chose the appropriate size - if heightened concern about leakage - as in a patient with previous chemoradiation, then a smaller catheter such as 14 Fr.)
- Silk suture size #0
- Chromic suture size 4-0 "double-armed" or dacryo (G-3) needle x 4
- 22-gauge spinal needle
- Voice prosthesis if requested
- Standard
- Medications (specific to nursing)
- 1% lidocaine with 1:100,000 epinephrine
- Codeine 30 mg PO may be given 30 minutes before procedure to suppress cough
- 1% pontocaine with epinephrine
- Viscous xylocaine 2%, 15 cc
- Dyclone 0.5%, 30 cc
- Prep and Drape
- Standard prep, 10% providone iodine
- Drape
- Head drape
- Towels to square off neck leaving face/mouth exposed
- Split sheet
- Drains and Dressings
- None
- Special Considerations
- None
- Positioning
- Supine (head of bed up) with neck minimally extended
- Have patient partially swallow Maloney dilator (between sizes #30 to #40). Secure the dilators so they are not swallowed entirely.
ANESTHESIA CONSIDERATIONS
- None (done under local anesthesia). This same technique can be used under general anesthesia.
OPERATIVE PROCEDURE
- Patient should rinse oral cavity with Dyclone 0.5%. Inject local anesthesia 1% lidocaine with 1:100,000 epinephrine into posterior tracheal wall. Place hollow Maloney dilator
- Place spinal needle through posterior tracheal wall impaling Maloney dilator 10 to 15 mm (average of 13 mm) inferior to the mucocutaneous junction of the tracheostoma. Ensure that the Maloney dilator has been emptied of mercury before using it for this purpose. Note the newer dilators do not contain mercury.
- Incise mucosa with #11 scalpel blade immediately adjacent spinal needle in a vertical direction. Employ 2 small, single-pronged skin hooks used to retract the mucosa and muscle laterally until the orange of the dilator is clearly seen.
- A hemostat is used to dilate this newly created TEP site and clear material off the Maloney dilator, permitting deeper placement of the single hooks to lift and separate mucosa of the esophagus.
- The Maloney dilator is then removed, permitting placement of a red rubber catheter (14, 16, or 18 gauge) into the esophageal lumen between the two single-pronged skin hooks. The skin hooks are then removed.
- An 0-silk tie is tightly secured around the red rubber catheter (to prevent reflux of secretions) and then taped around the neck.
POSTOPERATIVE CARE
- Leave red rubber catheter in for 1 to 2 weeks.
- Patient returns to speech therapy for placement of TEP prosthesis and voice therapy.
- If there is difficulty with TEP speech, consider trial of lidocaine injection. If a positive response to lidocaine occurs, then offer Botox treatment to pharyngeal constrictors.
GENERAL ANESTHESIA
- Alternative Approach Under General Anesthesia
- Indications for general anesthesia
- Patient request
- Need for another procedure such as concurrent esophagoscopy or concurrent botulinum neurotoxin injection to cricopharyngeus
- Anesthetic Considerations
- Full relaxation
- May use same technique as above
- Ciaglia Blue Rhino Percutaneous tracheostomy (SEE VIDEO ABOVE)
- General anesthesia using a Rusch tube through the tracheostome.
- Rigid esophagoscopy with a long 0 degree telescope. Through visualization through the tracheostoma, the transilluminated endoscope was visualized.
- Rotate the endoscope 180 degrees so that the short end of the bevelled rigid cervical esophagoscope abuts the anterior esophageal wall.
- Inject the tracheostoma with 1% lidocaine and 1:100,000 epinephrine at the planned site for the puncture; 1.3 cm from the muco-cutaneous junction.
- Using the Ciaglia Blue Rhino percutaneous tracheotomy set
- Puncture through the posterior tracheal wall under endoscopic visualization using a 15-gauge access needle; The distal long end of the esophagoscope is used to protect the posterior wall of the esophagus.
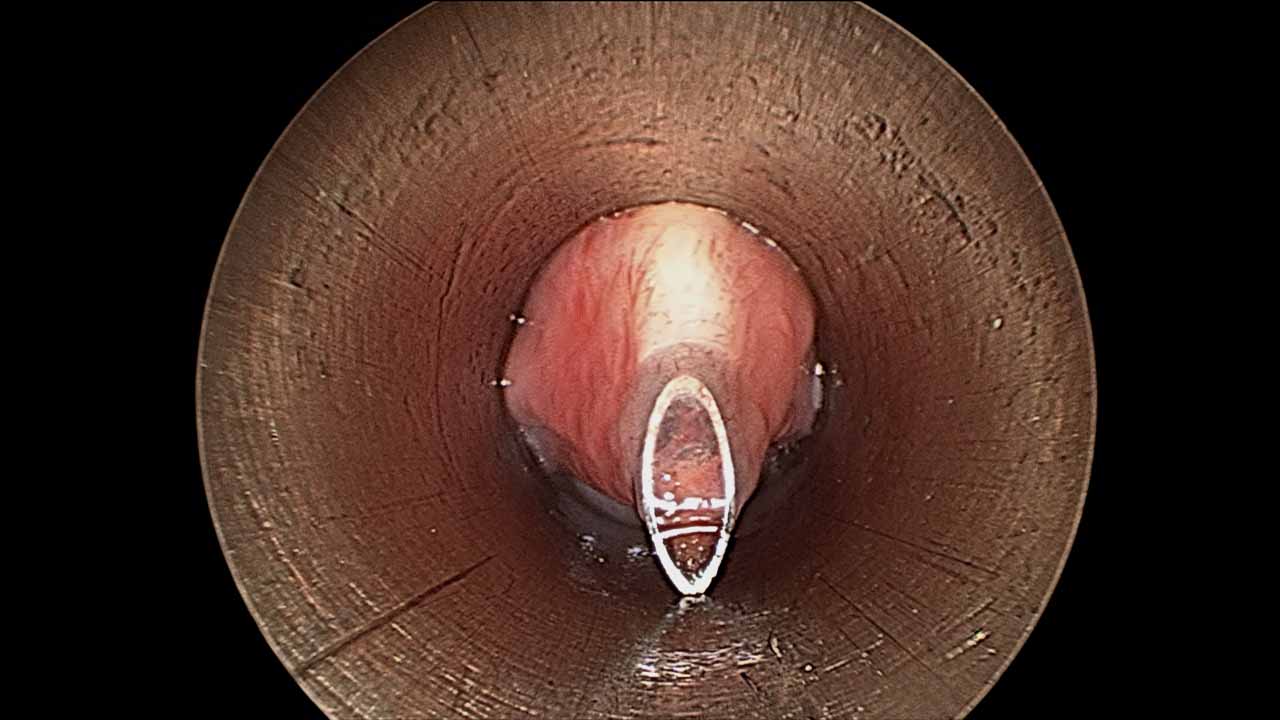
- Remove the needle leaving the needle sheath in place.

- Place guide-wire through the sheath
- Remove the access sheath.
- Dilate with percutaneous tracheostomy dilators over guide wire using the Seldinger technique.

- Remove the guide wire and dilator.
- Coat the Provox NiD voice prosthesis (ATOS medical AB, Horby,Sweden) with water soluble lubricant
- Place it through the TEP site using the Provox NiD inserter using a twisting motion under direct visualization through the endoscope.
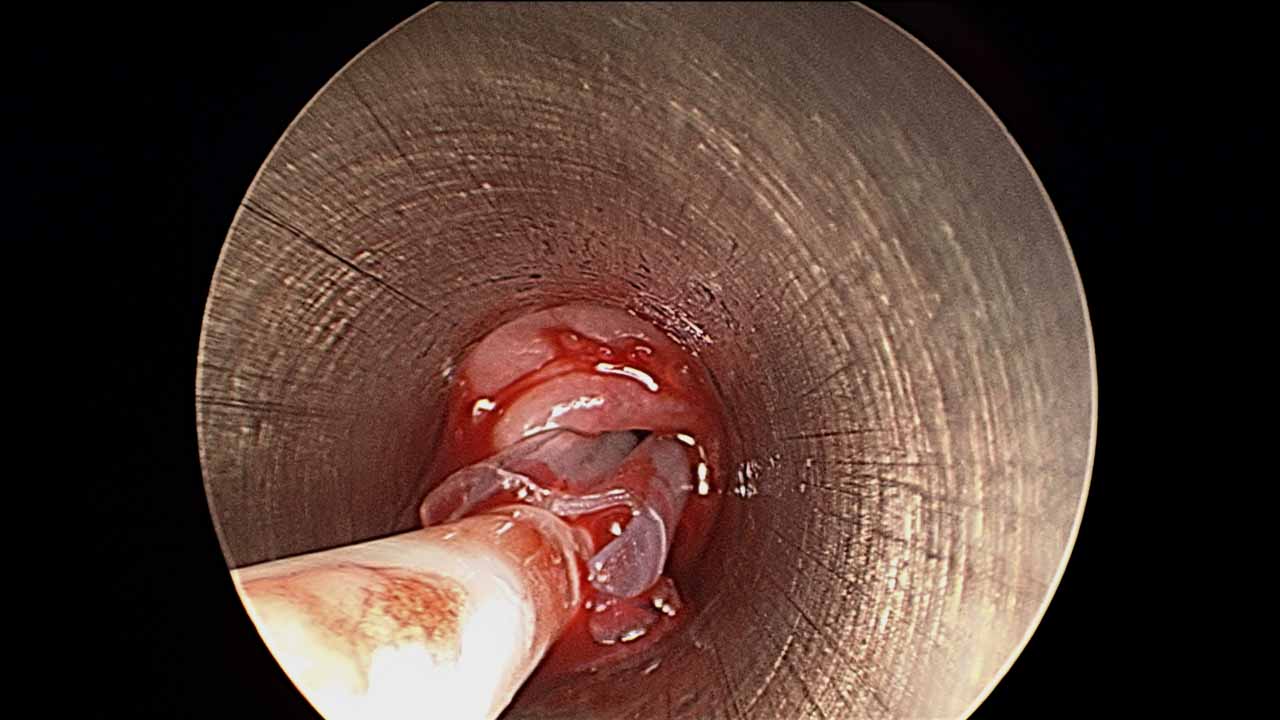
- The silicone valve flap and esophageal flange should be visualized in the anterior esophageal wall through the endoscope
-
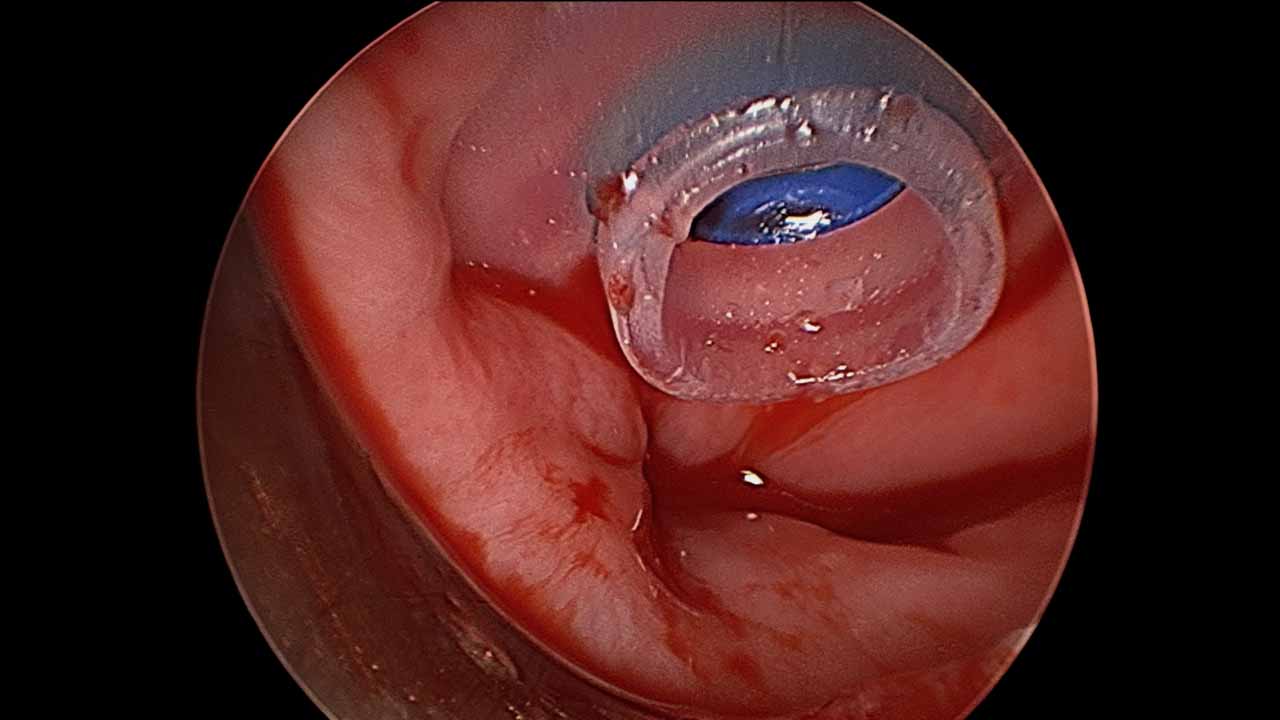
- If needed, place a single 4-0 Vicryl suture inferior to the prosthesis to prevent leakage of esophageal contents.
- Patients are NPO overnight and then start a liquid diet on post-operative day #1. This is advanced to a soft and then general diet over the next week.
- Ancillary Measures
- see: Botulinum toxin injection to cricopharyngeus
- see: Botulinum Neurotoxin A Injection
- Indications for general anesthesia
Sample dictation:
Patient was brought to main operating room with the bed turned 90 degrees from anesthesia. 2ml of 4% lidocaine was dripped into the laryngostoma for topical anesthesia and allowed time to take effect. A 5.0 MLT was inserted and general endotracheal anesthesia was induced. All pressure points were padded. A time out was performed. 1cc of 1% lidocaine with 1/100,000 epinephrine was injected for local anesthesia and vasoconstriction. This was allowed time to take effect. The cervical esophagoscope was inserted and rotated 180 degrees at the level of the laryngostoma. Under endoscopic visualization the guide needle and then wire were inserted. A Cook Ciaglia blue rhino dilator was inserted. This was previously marked for the appropriate diameter and length of TEP. The distance from stoma to esophagus was approximately *** mm. The appropriate size TE prosthesis was inserted over a guide catheter which was then removed. The TEP was seen to be well seated. (The insertion hole was deemed slightly large and a 4.0 vicryl suture was used in a vertical mattress fashion to decrease its diameter.) The TEP flange was oriented superiorly and a circumcervical 2.0 silk suture was used to loosely maintain this orientation. Photodocumentation was taken throughout. The patient tolerated this procedure well and was turned back over to the care of our anesthesia colleagues in stable condition.
REFERENCES
Hoffman HT, Baker SR. Tracheostoma diverticulum following tracheoesophageal puncture. Arch Otolaryngol. 1990;116:1074-1076.
Hoffman HT, Fischer H, VanDemark D, Peterson, KL, McCulloch T, Funk G. Botulinum injection after total laryngectomy. Head Neck. 1997;19:92-97.
Hoffman HT, McCulloch TM. Botulinum neurotoxin for TEP speech failure. In: . Blom E, Singer MI, Hamaker RC, eds. Tracheoesophageal Voice Restoration Following Total Laryngectomy. San Diego, Calif: Singular Publishing Group; 1998:81-85.
Malik T, et al. Surgical complications of tracheo-oesophageal puncture and speech valves. Curr Opin Otolaryngol Head Neck Surg. 2007 Apr;15(2):117-22.
Singer MI. The development of successful tracheoesophageal voice restoration. In: Deschler DG, ed. Otolaryngologic Clinics of North America: Voice Following Laryngeal Cancer Surgery. June 2004; vol 37, no 3: 507-518.
Singer MI, Blom ED. An endoscopic technique for restoration of voice after laryngectomy. Ann Otol Rhinol Laryngol 1980; 89:529-533.
Pagedar NA, Bayon R, Gudgeon J, Nelson RF, Van Daele DJ, Hoffman HT. Tracheoesophageal puncture with immediate prosthesis placement. Laryngoscope. 2014 Feb;124(2):466-8. doi: 10.1002/lary.23756. Epub 2013 Oct 15.