click on image above to enlarge; advance with cursor over border
return to: Subglottic stenosis or Granulomatosis with Polyangiitis (GPA)



Modified Operative Note
PREOPERATIVE DIAGNOSIS:
Subglottic stenosis
PROCEDURE PERFORMED:
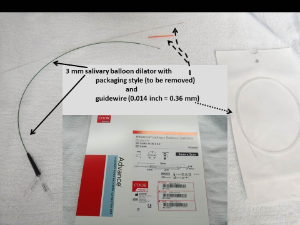
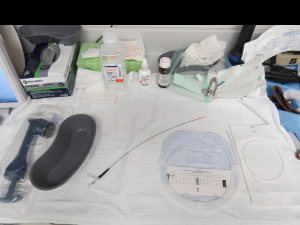
Trans-nasal laryngoscopy as well as trans-stomal bronchoscopy to the carina with retrograde dilation of subglottic stenosis using the advanced salivary balloon catheter with guidewire (3 cm length of balloon) with a 0.14 inch guidewire (0.36 mm diameter guidewire).
DESCRIPTION OF PROCEDURE:
Following identification of the patient, informed consent, and a brief timeout, initial anesthesia with bilateral superior laryngeal nerve blocks with injections in between the hyoid and the thyroid cartilage close to the greater cornu was done with 1 mL each with 1% lidocaine with 1:100,000 epinephrine.
Topical lidocaine, epinephrine to the nose and then to the tracheostome and then followed.
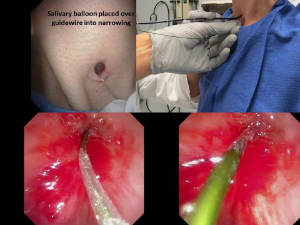
A view through the stomal retroflexed did show a pinpoint opening for the subglottis, which on initial efforts to cannulate were unsuccessful, but by using the guidewire with the "non-floppy end" bent at approximately a 45 degree angle with concurrent use of the flexible scope and the tracheotomy tube out, we were successful in inserting the 0.14 inch guidewire (0.36 mm) diameter over which the salivary balloon dilator (1 mm outer diameter) was then placed with the balloon positioned appropriately and inflated to 16 atmospheres (approximately 3.26 mm) and held for approximately 1 minute.
Re-inspection from above (trans-nasal laryngoscopy), showed appropriate placement with the tip of the catheter between the vocal cords (further supporting use of the superior nerve blocks to numb the neck appropriately), with deflation and then reinflation for another 30 seconds in a similar manner.
The #5 Jackson tracheostomy tube then replaced and tolerated the procedure well with review of the images with her identifying also her improved ease of phonation.
Suggestions given for continued frequent saline irrigations and tracheootomy changes as frequently as comfortable with use of voice as much as possible to continue to pass air through the narrowing.