Return to:
- 2016-2017 Temporal Bone Dissection Course for Iowa Otolaryngology Resident
- Temporal Bone Harvest
- Iowa Otolaryngology Resident Handbook
- Otology Neurotology Protocols
Content compiled by Xiaoyang Hua, MD, Department of Otolaryngology-Head and Neck Surgery University of Iowa Hospitals and Clinics
Purpose
The primary purpose of temporal bone drilling is to learn temporal bone anatomy. Figure 1 shows a near-complete cortical mastoidectomy (with mastoid tip intact), atticotomy, posterior tympanotomy, and dissection of the retrolabyrinthine and infralabyrinthine areas. For ease of description, we will describe the applied anatomy grossly based on superior, posterior and anterior dissections, although these dissections are usually carried out in a simultaneous fashion during temporal bone exercise.

Superior Dissection
The superior dissection should be started 1 cm above the temporal line (Figure 2A). The middle fossa plate (MFP) should be first identified in the squama of the temporal bone from the zygomatic root to the lateral sinus. The MFP is then followed medially to expose the tegmen. In a finished bone, the tegmen should be exposed from the zygmatic root to the sinodural angle (Citelli’s angle). Following the MFP is the safest way to expose the antrum. This technique is specifically useful when there is a low or sagging tegmen or a very dense Körner’s septum. If the tegmen in Figure 2A took a more inferior course, it would place the horizontal semicircular canal (HSCC) partially in the path toward the antrum. Drilling medially without following the tegmen would likely cause injury to the HSCC. Körner’s septum is the extension of the petrosquamous suture superiorly and tympanosquamous suture inferiorly. It forms the lateral wall of the antrum and separates mastoid cortex cells from petrous cells and the antrum (Figure 2B, KS partially opened). Körner’s septum is itself anatomically variable. Figure 2C demonstrates air cells lateral to KS. These cells can be mistaken for the antrum. Figure 2D demonstrates a very dense KS, which can be mistaken for the medial wall of the antrum. Following the MFP and tegmen anteriorly and medially will consistently lead to the antrum.


Posterior Dissection
The posterior limit of the dissection should demarcate the sigmoid sinus, which runs a posterolateral to anteromedial course. In most bones, the sigmoid sinus takes on a dark blue hue, but may be difficult to appreciate if the bone is very dense. Keeping a thin cortical layer over the sigmoid sinus and following its course inferiorly and anteriorly is the key to skeletonizing the sigmoid (Figure 3A). The distance between the sigmoid and the anterior structures including the posterior semicircular canal (PSCC) and the descendingfacial nerve is variable. Keep these structures in mind during the dissection, particularly in cases where the sigmoid sinus appears to be shifted anteriorly.
The Citelli’s angle (sinodural angle) is formed by the tegmen superiorly and the transverse sinus inferiorly (Figure 3B). The sigmoid sinus is the continuation of the transverse sinus at this point. Citelli’s angle can be easily skeletonized by placing the burr at the corner between the sigmoid and the tegmen and drilling in a medial to lateral direction. Skeletonizing the sinodural angle bevels the bone and improves access to deeper structures. Once Citelli’s angle has been skeletonized, Trautmann’s triangle is apparent. Trautmann’s triangle is formed by the superior petrosal sinus (SPS) superiorly, the sigmoid sinus and the posterior fossa plate posteriorly, and the posterior semicircular canal (PSCC) anteriorly (Figure 3B and C). Trautmann’s triangle contains the retrolabyrinthine tract that leads to the petrous apex, the endolymphatic sac and the vestibular aqueduct (Figure 3B and C). The endolymphatic sac is a triangular structure situated inferior to the Donaldson’s line (an imaginary line running parallel to the HSCC, Figure 3B). The location of the endolymphatic sac is variable. The key to find it is to follow a very thin layer of posterior fossa plate to identify the thickened posterior fossa dura.
The digastric ridge (DR) is situated lateral to the sigmoid sinus (Figure 3A). It runs in a posterior to anterior, lateral to medial direction and meets the facial nerve at the stylomastoid foramen. The DR can be safely identified posteriorly using a cutting burr and can then be followed anteriorly. As it approaches the bony portion of the external auditory canal, a diamond burr with copious irrigation should be used so as not to injure the facial nerve or violate the EAC. The yellow-brown colored aponeurosis can be easily appreciated (Figure 3 A), indicating its proximity to the stylomastoid foramen and FN. As long as a thin bony plate is kept on the digastric ridge, the FN is safe. The mastoid tip lateral to the DR can be safely amputated.

Anterior Dissection
The anterior limit of dissection focuses on thinning the EAC wall, and identifying the chorda tympani, facial nerve, and the facial recess. In the meantime, the EAC should not be shortened or penetrated. Careful bone reading is the key to successful anterior dissection. Rotate the bone for en face bone reading and use higher magnification for deep dissection.
The anterior dissection is started by drilling a shallow groove posterior to the Spine of Henle. The groove should extend from the root of the zygoma to the mastoid tip (Figure 4A). Keep the spine of Henle intact as a landmark to avoid shortening the EAC. The posterior EAC wall is thinned using long steady strokes that parallel the descending facial nerve. The superficial dissection can be carried out using large cutting burr. A 3-4mm diamond burr with adequate irrigation should be used when the dissection is carried medially and close to the facial nerve. A finished bone should have a two planar view, which is formed by the thinned EAC and the saggital plane tangential to the FN (Figure 4B).
Three important landmarks guide the anterior dissection: the cortical plate of the EAC, the incus pointer and the descending FN. The EAC wall should be thinned until the cortical plate is identified. The drilling is then carried on medially following the plate. In the meantime, the dissection should be directed at the incus pointer, which bisects the facial recess (Figure 4C). The FR is defined by the incus buttress superiorly, the chorda tympani anteriorly and the facial nerve posteriorly. As shown (Figure 4C), the FR is widest (and safest for drilling) when it is closer to the incus pointer (this is why the buttress should be kept very thin during posterior tympanostomy). The third landmark is the descending facial nerve.
The course of the descending portion of the facial nerve is just medial to an imaginary line connecting the midpoint of the HSCC and the anterior extent of the digastric ridge (DR). Dissect out the HSCC and DR, keep the estimated course of descending FN in mind during anterior dissection, and adjust your drilling to avoid injury to the FN.
During anterior dissection, careful examination of the temporal bone with sufficient magnification is the key to identifying the descending FN. In preserved bones, the facial nerve fallopian canal is often a pearly white (Figure 4D) or salmon (Figure 4B). In living specimens, it is salmon (the vessels give it color). Additionally, the peri-facial cellscan sometimes be seen. This tract consists of cells surrounding the fallopian canal (Figure 4C) and is anatomically variable. While in some bones, the tract is readily appreciable and the fallopian canal can be somewhat visualized through the woven perifacial tract, some have very limited cells around the fallopian canal. As such, do NOT always expect peri-facial cells around the fallopian canal.
The chorda tympani usually takes off from the FN slightly before the stylomastoid foramen (Figure 4B and C) (This anatomy is quite variable). It then runs superiorly, anteriorly and laterally to the FN. Careful bone reading (en face, high power magnification) is the key to identifying the chorda. A sensory branch of the facial nerve can be often encountered when dissecting anteriorly (Figure 4D). Following the sensory branch may help identify the chorda tympani and FN but this should not be used as a general rule (Ref).
Once the FR and incus buttress have been well defined, open the FR slightly inferior to the incus pointer by using a 2mm diamond burr (the distance between the FN and the chorda at where it enters the middle ear is 2.9 +/- 0.7mm (ranges from 1.7-4.5mm, Figure 4F, Ref). Keep the buttress thin but intact and use the size of the burr to estimate the thickness. A sentinel cell is usually encountered during this step. The facial recess should then be widened to ensure full visualization of the round window and promontory (you may need to rotate your bone). The bony lip medial to the FN and lateral to the sinus tympani (^^ in Figure 4E) should be drilled in a lateral to medial direction, which will help expose the RW. Watch the shaft of the drill and don’t let a running drill pass through the facial recess.


Epitympanum
Removal of the lateral wall of the epitympanum and the air cells of the zygmatic root help expose the incus and malleus head. It is critical that burr never come in direct contact with any part of the ossicular chain as doing so will result in irreversible high frequency sensorineural hearing loss. The tegmen and superior EAC wall should be kept intact and the medial-most lip (the scutum) should not be violated. Please keep in mind that the tegmen is lower anteriorly towards the zygomatic root. For this step, 1) use appropriately sized burrs (cutting or diamond burr), 2) carry out the dissection in a medial to lateral direction (drill away from the ossicles, Figure 5A) and 3) use sufficient magnification.
The cog divides the epitympanum into anterior and posterior compartments and is a bony septum anterior and superior to the head of the malleus. It runs from the tegmen and to a point just superior to the cochleariform process (Figure 5 C, D and E). An atticotomy does not offer full access to the cog or the anterior epitympanum (Figure E) until the incus and head of malleus are removed. Removal of the cog will allow full access to anterior epitypanum (also called the supratubal recess, STR, Figure 5 B and H). The geniculate ganglion is found medial to the STR (Figure 5D).
Prussak’s space is defined by the scutum and the pars flaccida laterally, the malleus neck medially, and the lateral process of the malleus inferiorly (Figure 5F and G). Atticotomy by itself does not provide sufficient surgical access to Prussak’s space. If disease is suspected in this area, removal of the incus and head of the malleus facilitates access to Prussak’s Space (Figure 5H). Surgically, the Prussak space can be accessed transcanally as well. The scutum is important in preventing the formation of a postoperative retraction pocket (Figure 5H). As such, the scutum should be left intact and a scutum damaged by cholesteatoma should be reconstructed.
Posterior tympanotomy allows partial access to the stapes. If the entire stapes needs to be exposed, a posterior tympanotomy plus removal of the incus, incus buttress and the malleus head (Figure 5 I and J) will facilitate this. The incus buttress holds the ligament to the short process of the incus. If the incus has been removed, the incus buttress no longer serves an anatomic function.

Facial Nerve Decompression
The tympanic and descending segments of the FN can be decompressed in the temporal bone lab (Figure 6A and B). To decompress the facial nerve from the cochleariform process (CP) to the stylomastoid foramen (SMF), the dissection of the facial recess (FR), careful bone reading, and sufficient magnification are the keys. Do not attempt to drill any part of the facial nerve course that is mobile on gentle palpation. The largest available diamond burr with copious irrigation should be used. The goal in drilling along the course of the facial nerve is to leave an eggshell-thin layer of bone on over the FN, which can then be unroofed using a Rosen needle, Fisch dissector or other fine, probing instrument. For mastoid segment extending from the SMF to the facial recess, bone should be sculpted along the posterior aspect of the fallopian canal to prevent damage to the chorda tympani (Figure 6B). At the facial recess, drilling should be directed laterally (atop the nerve) to protect the HSCC (Figure 6B). For the segment extending from the cochleariform to the FR, about 30% have fallopian canal dehiscence. If there is dehiscence, the bony wall is usually thin enough to be removed without drilling (Per Dr. Hansen). Otherwise, the drilling should be directed anteriorly and inferiorly to protect the HSCC (House Manual).
Clinically, decompression of the segment from the 1st genu to the CP (tympanic segment) is performed via MCF approach at UIHC (Figure 15B and C). In temporal lab, this segment can be decompressed by drilling between the ossicles and the fallopian canal (ref both House T Bone Dissection Manual and Dr. Jack Pulec’s Video, Figure 6A). However, this is a difficult maneuver due to lacking of adequate visualization.

Retrolabyrinthine, Infralabyrinthine, Retrofacial Cells
Jugular bulb, Supra-antero Labyrinthine Tract, Solid Triangle, and Subarcuate Artery
- Retrolabyrinthine tract (*, Figure 7A): the cell tract posterior to the labyrinth. This tract runs along the tegmen (superior), posterior fossa plate (posterior) and superior petrosal sinus and connects with the petrous apex.
- Infralabyrinthine cells(**, have already been removed in Figure 7A): the cells surrounded by the labyrinth (superior), the digastric ridge (inferior), the FN (anterior), the sigmoid sinus and endolymphatic sac (posterior) and the jugular bulb (medial).
- Retrofacial cells (^^, Figure 7A): the cells between the FN (lateral) and jugular bulb (medial)
- Supralabyrinthine tract (#, Figure 7B): the cell tract between the SSCC and the middle fossa plate; variable.
- Anterolabyrinthine tract (##,Figure 7B): the cell tract surrounded by the SSCC, the tegmen, and tympanic FN. The labyrinthine segment of the FN is also in this region.
- Solid triangle (Figure 7B): surrounded by the SCCs.
- Subarcuate artery (Figure 7B): exits the solid triangle and provides blood supply to the mastoid

Labyrinthectomy
Understanding the relationship between the SCCs (Figure 8A, B and C) is the key to labyrinthectomy. Figure 8A shows the relationship between the SCCs. Figure 8B and C show the common crus which leads to the utricle. The vestibular aqueduct is located medial to the common crus (it bifurcates and connect with the utricle and saccule individually, Figure 8D).
- Perilymph circulation: the perilymph chamber of the vestibular system connects with the scala vestibuli. The scala vestibuli connects to the scala tympani at the helicotrema. The scala tympani then connects with the subarachnoid space through the cochlear aqueduct.
- Endolymph circulation: the endolymph chamber of the cochlea (scala media) connects with the saccule via the ductus reuniens. The saccule then connects with the endolymphatic sacthrough the vestibular aqueduct. The endolymph of the utricle and semi-circular canals also connect to the endolymphatic sac (Figure 8D demonstrates that the vestibular aqueduct splits into two branches behind the common crus which connect with the scaccule and utricle, respectively).


Translab and IAC
For a translabyrinthine approach, identify the following structures to estimate the location of the IAC after labyrinthectomy: EAC, subarcuate artery, SSCC ampulla, PSCC ampulla, jugular bulb and vestibule.
- The IAC runs in a direction that parallels the EAC
- A line drawn through the subarcuate artery and the SSCC ampulla marks the superior border of the IAC. There is usually very thick bone between the MFP and the superior border of the IAC. This is the place where the superior trough should be.
- The PSCC ampulla marks the inferior border the IAC; there is usually very thick bone between the inferior border of the IAC and the jugular bulb. This is the place where the inferior trough should be (see below)
- The vestibule marks the lateral end of the IAC (the fundus)
Once the borders of the IAC are estimated, there are two ways to find the IAC (Figure 9A and B, Figure 14C and D):
- Lateral approach: in this approach, identify the IAC from the fundus by drilling the medial wall of the vestibule first. Watch for color change while drilling to identify the transverse crest then the IAC. Once the IAC is identified, drill medially towards the porus to define its course. A thin layer of bone should be kept atop. The bone superior and inferior to the IAC is then drilled to achieve 270-degree exposure.
- Medial approach: in this approach, first drill along the posterior fossa plate to identify the IAC medially (around the porus). Then define the course of IAC by drilling from the porus to the fundus.


Several points no matter what approach is used:
- Superior drilling: Superior drilling is performed to develop the superior trench. All the bone between the IAC and the MFP can be removed. This maneuver is safe as long as a thin layer bone is kept intact along the IAC.
- Superior-anterior drilling: The labyrinthine segment of the FN, the geniculate ganglion, and the tympanic segment are located in this narrow area making the dissection somewhat challenging. It is possible that the edge of the burr could accidently injure the tympanic segment of the FN from medial side while following the labyrinthine segment anteriorly, especially when it is approaching the geniculate ganglion. The following strategy may help. First, remove the bone between the MFP and the tympanic segment of the FN. This is relatively safe as the labyrinthine segment is deeper than this plane; only the tympanic segment is at risk and thus needs to be watched closely during drilling. This step will help define the anterior end of the labyrinthine segment (geniculate ganglion). Second, identify Bill’s bar to identify the beginning of the labyrinthine FN. Third, remove the bone in between. During this step, drill superiorly (between the MFP and the labyrinthine segment) is a safe maneuver to define the entire course of the labynrinthine segment as it is away from the tympanic FN.
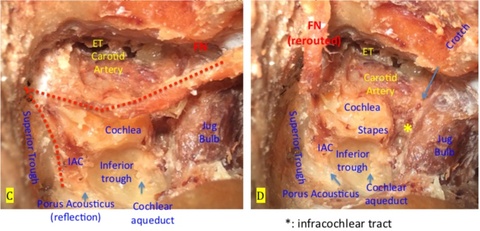
- Inferior drilling: this is to develop the inferior trough. During this step, keep a thin layer of bony plate atop the IAC and Jugular bulb is the key. The cochlear aqueduct can be seen during this step (Figure 14C and D). From this vantage point, the cochlear aqueduct can be seen running from the jugular foramen to the medial wall of the basal turn of the cochlea (the stapes and oval window are on the lateral wall of the basal turn).
- Posterior drilling to remove the bone between the IAC and PCF. This step is safe as long as a thin layer of bone is kept intact on the IAC and posterior fossa. Once the porus acousticus is reached, carry on drilling superiorly along the superior petrous sinus which will lead to the petrous apex.
Extended Facial Recess
After posterior tympanotomy, the chorda is transected along the FN. The annulus is then identified. Follow the annulus and remove all the bone anterior to the FN, inferior to the annulus plane, and lateral to the jugular bulb and the ICA.

Posterior Exposure of the Jugular Foramen
Mastoid-neck Approach/Mastoid Preparation
- Includes Mastoid- neck, with or without partial rerouting of the FN.
- Exposure of the jugular bulb facilitated by first performing an extended FR and removal of the bone in the infralabyrinthine and retrofacial areas (Figure 11A). The mastoid tip lateral to the digastric muscle (Figure 11 A, the bone pointed by the arrows) is then removed. The digastric muscle and the aponeurosis are then freed posteriorly and retracted anteriorly (Figure 11A and B). The bone between the descending FN and the sigmoid sinus is then removed to expose the jugular bulb (Figure 11B). While this approach can expose the jugular bulb, its anterior wall, which is adjacent to the ICA, is still blocked by the FN. As such, this approach cannot be used if the ICA needs to be accessed (Ref Otologic Surgery).
- Partial facial nerve rerouting: the Fallopian canal is unroofed from the second genu to the stylomastoid foramen. The FN is then freed using right angle hook or Fisch dissector. The FN along with the digastric muscle and parotid are then rerouted from the second genu (Figure 12).


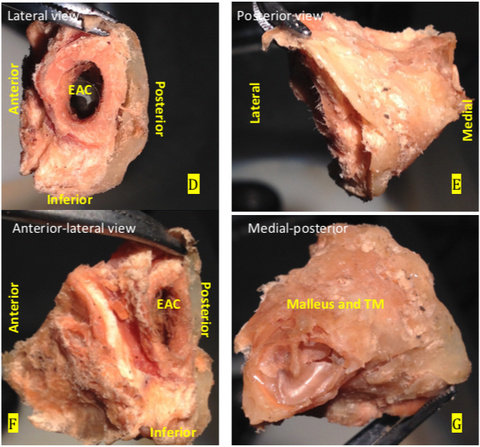
Partial Temporal Bone Resection
After mastoidectomy and atticotomy (Figure 13A and B), extended facial recess (Figure 13 C), the IS joint is dislocated, incus and buttress are removed, malleus head is amputated. Next, carry the dissection from the zygomatic root towards the glenoid fossa of the temporalmandibular joint superiorly and the parotid inferiorly (Figure 13A). At this point, the only place holding the EAC is the anterior wall of the EAC (lateral wall of the Eustachian tube). The dissection is to insert a small diamond burr into the Eustachian tube and drill laterally to free its lateral wall (do not drill medially as it is the ICA). The surrounding tissue is then dissected away from the EAC. Gently rock the EAC to remove it en bloc (Figure 13D, E, F and G).

Canal Wall Down, Subtotal Petrosectomy, Facial Nerve Re-routing and Jugular Bulb Anatomy
- Canal wall down mastoidectomy includes a cortical mastoidectomy, atticotomy and removal of the posterior EAC wall. The anterior buttress should be flat while the posterior buttress should be at the same level as the EAC floor. All bone lateral of the FN between the tegmen and EAC floor should be removed. All middle ear contents are removed including the TM and the ossicles. A thin layer of bone should be kept on the FN.
- Subtotal petrosectomy: after performing a canal wall down mastoidectomy (Figure 14A) and FN decompression (mastoid and tympanic segments, Figure 14A), drill down the inferior EAC wall until jugular bulb is encountered. Next, drill down the anterior wall to expose the TMJ. Drill out the ICA (Figure 14B) (A translabynthine exposure was performed in this bone to demonstrate the FN course. This is for illustrative purposes only and is not a part of the Subtotal petrosectomy).
- Facial nerve rerouting from the 1stgenu (Figure 14C and D)
- Open the jugular bulb to identify the IPS (inferior petrosal sinus) and pars nervosa (Figure 14E, dotted line demoes the pars venosa). The jugular foramen is divided by the jugular process into pars nervosa (anterior) and pars venosa (posterior). The pars nervosa contains the CN IX and IPS and the pars venosa contains the CN X and XI, the jugular bulb, and the posterior meningeal artery. The inferior petrosal sinus is located between the CN IX and X and may have single or multiple venous channels.


MCF Approach
After performing a craniotomy, elevate the dura from the squama to the MCF floor. Dissection should be carried out from lateral to medial and from posterior to anterior to spare the GSPN and the lesser petrosal nerve, which is located anterior and lateral to the GSPN. Recognizing the following anatomic landmarks is the key (Figure 15).
- Foramen spinosum (Figure 15A): the outermost lateral structure in the MF through which the middle meningeal artery, a branch of the internal maxillary artery, enters the middle fossa. It has two branches, the anterior and posterior branches. The sensory branch of the V3 that returns to the dura also transits foramen spinosum.
- GSPN (Figure 15 A-C): after taking off from the geniculate ganglion, it runs in the sphenopetrosal groove, courses between the foramen ovale and the foramen lacerum where the deep petrosal nerve from the pericarotid plexus (sympathetic components) join the GSPN. It then enters the foramen lacerum, transits the pterygoid canal and enters sphenopalatine fossa through the vidian canal. The Internal carotid is underneath the GSPN (Figure 15B).
- Lesser petrosal nerve: parasympathetic fibers from the CN IX (Jacobson plexus), exits from foramen ovale. It courses lateral to the GSPN.
- Arcuate eminence: The arcuate eminence is NOT a consistent landmark for identifying the SSCC (Figure 15 A and B to show the blue lined SCC is posterior to the arcuate eminence)
- Kawase area: defined anteriorly by V3, laterally by GSPN and posteriorly by IAC (Figure 15 B and C).
- Glasscock’s triangle: defined by V3 anteriorly, GSPN medially and an imaginary line from foramen spinosum to the origin of the GSPN.
- Petrous carotid is just under the GSPN (see Figure 15B and C).
Three ways to find the IAC
- Fisch method: 60 degrees from the arcuate eminence. Drill medially to identify the ICA and then move laterally to the geniculate ganglion (GG)
- Garcia method: Identify the arcuate eminence and the GSPN then drill along the angle bisector formed at the intersection of the line running through these structures.
- House method: Identify the geniculate ganglion first. Next, identify the labyrinthine segment of the FN. Follow the labyrinthine segment medially and posteriorly to identify the IAC.
Pearls
- Raise the dura medially until the MMA and the foramen spinosum are encountered anteriorly and the superior petrosal sinus is identified posteriorly. Ligate the MMA. Then raise the dura from the middle fossa floor in a posterior to anterior direction to protect and identify the GSPN and the lesser petrosal nerve. Once these two nerves are identified, continue elevating the dura medially and posteriorly to the superior petrosal sinus. This maneuver can be practiced in the temporal bone lab as long as the dura has been left intact during the preservation process.
- To find the IAC, identify the GSPN and the arcuate eminence, which form an angle of about 120 degree (Figure 15A). If using Fisch’s method, find IAC medically as this will stay away from the SSCC and cochlea. Continue dissecting laterally toward the arcuate eminence along the superior petrosal sinus until the IAC is identified. Sometimes, the subarcuate artery is encountered. If using Garcia method, try to find the IAC medial as well. The IAC is slightly located lateral to the angle bisector (Figure 16A).
- Blue line the SSCC: the subarcutate eminence is NOT a consistent landmark for identifying the SSCC. To “blue-line” the SSCC, use low speed, sufficient magnification and drill in a direction perpendicular to the superior petrosal sinus and around the arcuate eminence with copious irrigation, and watch for the very subtle color change (Figure 15B and C, Figure 16B).
- Once the IAC is identified, drill along the IAC laterally toward the junction between the GSPN and the arcuate eminence. Drilling should remain along the roof and posterior wall of the IAC with a thin bony cortex left intact. The purpose is to protect the cochlea, which is VERY close to the IAC anteriorly (see Figure 15B and D, Figure 16 is to show an opened cochlea) and is almost at the same level as the IAC. In OR, a measuring needle can be used to estimate how far the drilling is from the cochlea which is just 1-2mm anterior to the IAC. In addition, be aware of any color change, as the cochlear capsule is yellow in color (Figure 15B and D, Figure 16C and D)
- Once the labyrinthine segment and the Bill’s Bar are identified, use a small diamond burr to drill along the labyrinthine segment of the FN until the geniculate ganglion has been identified.
- The geniculate ganglion is at the distal end of the GSPN. It is not always covered by bone!



Cochleostomy
- About 30% of cochlear implants are performed through a cochleostomy while the remaining 70% are performed though the round window (per Dr. Hansen). As such, cochleostomy may not be required for CI
- Cochleostomy, if performed, should be anterior and inferior to the true RW membrane. If the cochleostomy is too far superior, it will enter the scala media. If it is too far inferior, it will enter the hypotympanic air cells.
- In Figure 17, the cochleostomy indicated by the red arrow is too far superior. Performing a cochleostomy at this location is a technical error. The more inferiorly place cochleostomy indicated by the yellow arrow is too far anterior. Ideal placement of a cochleostomy is between the round window and the yellow arrow right on anterior-inferior edge of the round window
- Cochleostomies sometimes technically challenging as in cases where the round window niche is hidden under the pyramidal process, and in those who have post-meningitis ossification. In these situations, a cochleostomy may be performed in the following locations:
- Through promontory to enter the scala tympani
- Through scala vestibuli if scala tympani has been completely obliterated
- CWD mastoidectomy followed by modiolus approach

How to Drill
- Posture: thigh parallel to the floor, shoulders back, neck relaxed with head squared over the shoulders.
- How to hold the drill:
- Hold the drill like a pencil. Holding the hand piece closer to the burr improves control, but may sacrifice balance.
- Always fulcrum! Never float your hand while drilling
- Rest your wrist or anchor the 4th and 5th digits on the adjacent structures (bone or the dissecting bowl) to stabilize the drill (Watch Dr. Gantz's pinky stabilization).
- Burrs:
- Cutting and diamond
- Use the largest burr possible, but not one that is so large that it inadvertently drills adjacent structures.
- Use the side of burr instead of the tip. It is more difficult to control the drill when drilling with the tip and visualization is suboptimal.
- Stryker burrs: Diamond (fine, regular, and coarse), Cutting (multi-flute vs. 2 flute)
-

- Swipes
- Drill strokes should be in one direction instead of back and forth. Use long, steady strokes.
- Start the drill before touching the bone
- The direction of drill strokes should be the same direction that the burr rotates. This prevents the drill from skipping. When drilling in close proximity to vital structures, drill away from them instead of toward them regardless of which direction the burr is rotating. It is better for the drill to skip than to accidentally damage a vital structure.
- Read the bone!!!
- Should not drill if the bone has not been read or cannot be read (Never drill blindly unless you are an expert)
- Adjust the microscope and position of the bone to read it en face.
- Saucerization allows better bone reading.
- Suction and irrigation should remove the bone dust efficiently and should not interfere with bone reading.
- Adjust your drilling— location, force applied, direction, speed, etc. This is an exercise in hand, foot and eye coordination!
- Suction and Irrigation:
- Irrigation should be sufficient to effectively cool the bone and remove the dust. Frictional heat is dangerous to the facial nerve. Do not flood the field with irrigation as this decreases visualization.
- The suction should be placed where the dust and water can be removed effectively. It sometimes helpful to the use the suction irrigator to shield vital structures from the drill in case the drill accidentally slips.
- How to set up the microscope
- Don't wear glasses if possible. If you must wear glasses, fold the eye relief outward to minimize the distance between glasses and the eyepiece.
- Adjust the distance between the two eyepieces and set the diopters of both eyepieces at 0
- Set magnification to 40X and adjust the scope on a towel by using focus knob only
- Switch magnification to 6X and adjust the diopter of the eyepieces individually to obtain the sharpest image
- Remember your diopter readings for future use (distance and focus)
References
Eshraghi AA1, Buchman CA, Telischi FF. Sensory auricular branch of the facial nerve. Otol Neurotol. 2002 May;23(3):393-6.
Temporal Bone Dissection Guide first version, by John K. Niparko, MD
Temporal Bone Dissection Guide, by House Ear Institute
Acknowledgements: The author would like to thank Bruce Gantz MD, Marlan Hansen MD, Daniel Sun MD, and Joshua Tokita MD for editing and reviewing this manual.

























