General Considerations
- Indications
- If harvested to the midline, the temporoparietal flap provides a thin well-vascularized fascial flap that is easily rotated to cover orbital defects extending to the nose, cheek defects extending to the oral commissure, and intraoral defects over the body of the mandible.
- The flap readily accepts a skin graft and may be harvested with a hair-bearing skin paddle. If required, the flap may be harvested with an outer table cranial bone component as a composite flap. Within head and neck reconstruction, the flap probably has been used most extensively in orbital and maxillary reconstruction. The flap may be used as a turndown flap to cover auricular skin defects or to cover the cartilaginous framework of a reconstructed ear. This flap may also be harvested as a free flap for use in remote sites.
- Contraindications
- Prior sacrifice or injury to the superficial temporal artery system would contraindicate the use of this flap. This can be evaluated with a Doppler in the clinic if there is a question regarding the integrity of this vessel.
- Prior surgery or trauma in the temporoparietal area that may have disrupted this fascial layer would contraindicate its use. Harvest of the flap requires a vertical incision from the helical root up to approximately the midline, usually terminating in a "V" to improve anterior and posterior exposure. This incision is camouflaged well in patients with thick hair.
- In the bald patient or the patient with a receding hairline, this incision would be much more visible and be a relative contraindication to flap harvest. This would be a significant consideration in the younger male with early onset of male pattern baldness.
- Prior radiation to the temporoparietal area is not an absolute contraindication. However, if there is evidence of significant tissue injury and fibrosis, it would be wise to use an alternative. Prior radiation to the donor site will also increase the potential for scalp wound healing complications after flap elevation.
- Pertinent Anatomy
- The temporoparietal fascia is continuous with the SMAS inferiorly and the galea superiorly. The transition from temporoparietal fascia to galea occurs in the region of the temporal line. Above the temporal line, the fibrous connections between the dermis and fascial layer become more numerous making dissection somewhat more tedious.
- The temporoparietal fascial plane lies between the subcutaneous tissue and superficial layer of the deep temporal fascia below the temporal line. Above the temporal line, the galeal layer lies between the subcutaneous tissue and the subgaleal fascia, also called the loose areolar tissue component of the pericranium.
- The superficial temporal artery runs within the fascia in an axial pattern. The superficial temporal veins tend to run on the outer surface of the fascial layer, and they are much more prominently visualized during harvest.
- Anteriorly, this fascial plane receives blood from the supraorbital and supratrochlear vessels (these of course are not important for the laterally-based temporoparietal flap). A well-defined fascial plane with a visible axial blood supply is present for approximately 12 cm above the root of the helix. Above this point, the temporoparietal flap begins to fuse with the subcutaneous tissue, making dissection difficult but not impossible.
- The temporoparietal-galeal flap may easily be harvested to the midline of the scalp.
- Anteriorly, the frontal branch of the facial nerve runs on the undersurface of the temporoparietal fascia. This structure delineates the anterior margin of the flap.
Preoperative Preparation
- Evaluation
- Detailed history and physical examination: The physical examination may include use of a Doppler to map out the course of the superficial temporal artery.
- History of familial baldness
- Potential Complications
- Alopecia along the incision line is the most frequent complication, and patients should be aware of this. The affected areas may be excised at a later time if it is particularly noticeable.
- Injury to the frontal branch of the facial nerve is a potential complication.
- The vascularity of the scalp edges may be tenuous following the elevation of a large flap. This may result in wound breakdown and require healing by secondary intention.
- Although this flap is well vascularized and robust, dissection of the flap is tedious, and great care must be taken in separating the subcutaneous tissue from the underlying axial vascular supply. If the superficial temporal artery or veins are injured during elevation, the flap may not be useable. Great care must be taken in the initial elevation of skin flaps away from the temporoparietal fascia to develop the correct level of dissection and avoid injury to the vasculature. Dissection immediately deepto the hair follicle roots (if present), delineates a proper plane and serves to protect the hair roots.
Nursing Considerations
- Room Setup
- Instrumentation and Equipment
- Standard
- Special
- Varidyne vacuum suction controller
- Nerve stimulator control unit and instrument
- Doppler probe and box
- Dermatome (available only)
- Medications (specific to nursing)
- 1% lidocaine with 1:100,000 epinephrine
- Antibiotic ointment (see Antibiotic Prophylaxis in Head and Neck Surgery protocol)
- Prep and Drape
- Standard prep, 10% providone iodine
- Drape
- Head drape
- Towels to square off incision line
- Plastic drape (1010 drape) to cover nose and mouth (depending on extent of defect being reconstructed)
- Split sheet
- Drains and Dressings
- Varidyne vacuum suction drain: 7 mm or 10 mm, x 2
- Antibiotic ointment to suture line
- Special Considerations
- Skin graft may be necessary
- If calvarium harvested, order
- Hall Micro Sagittal Saw Tray (Pneumatic)
- Midas Rex Drill Tray with burr
- Nasal Sharp Tray
- Bien Otologic Electric Drill Tray
- KLS Oto Trauma Implant - Instrument Tray
- Bone wax
- The surgeon should use loupe magnification for elevation of this flap.
- The flap dissection initially, during elevation of the skin flaps off of the temporoparietal fascia and galea superiorly, may be rather bloody.
- Facial nerve stimulator
- The recipient area should be prepped as needed. The entire lateral face is prepped, and the hair is shampooed with prep solution to allow easy access to the entire lateral scalp. The hair is parted along the intended incision lines. No hair is shaved. Rubber band pigtails along the incision line keep hair out of the wound.
Anesthetic Considerations
- General
- The patient is supine on the operating table in the head lateral position. A Mayfield headrest allows the surgeon to be closer to the field and is recommended.
- In general, the patient is orally intubated with the tubing running along the chest.
- Specific
- The patient should not be paralyzed during the procedure. After the flap has been elevated and is ready to be inset, the patient may be paralyzed if this facilitates the anesthetic care of the patient.
Operative Procedure
- With the nerve stimulator on 10, identify the approximate course of the frontal branch of the facial nerve transcutaneously.
- Vertical incision from just anterior to the helical crus directed vertically approximately 12 to 14 cm. A horizontal incision to form a "T" at the top of the vertical incision may facilitate anterior and posterior exposure. This may also take the form of a "V." The incision should start in the area about 2 cm above the helical root. The temporoparietal fascial plane is easiest to identify in this area. The vertical incision may extend superiorly in a "piecemeal" fashion so that it is made with the temporoparietal fascia under direct vision.
- The incision should be carried down to the temporoparietal fascia. This plane is best identified by first identifying the plane containing the superficial temporal vessels several centimeters above the ear as above.
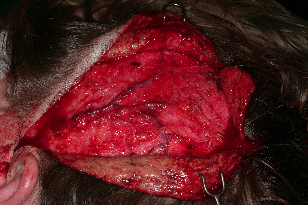
- Following definitive identification of the temporoparietal fascia, the overlying flaps are elevated off of it.
- The best way to identify the temporoparietal fascia is to stay in the plane containing the vessels. At times, the dissection will be immediately below the hair follicles.
- Elevation of the overlying skin and subcutaneous tissue is extremely tedious. It cannot be done rapidly without injuring the underlying flap.
- As dissection extends anteriorly, look for the facial nerve on the undersurface of the temporoparietal flap and identify it with the help of the nerve stimulator. Once it has been identified, do not dissect the temporoparietal fascia below that level.
- The plane of dissection will become more superficial as dissection is carried out superiorly. The fibrous attachments of the fascial layer and the overlying subcutaneous tissue will also increase above the temporal line. Dissection near the midline 12 to 14 cm above the helical root may become very tedious.
- After the desired size flap has been exposed, it needs to be elevated. This is much faster and simpler than exposing the fascia.
- Beginning superiorly, simply elevate the vascular fascial flap off of the pericranium. This is done in the avascular plane of the subgaleal fascia. Below the temporal line, the fascia is elevated off of the superficial layer of the deep temporal fascia. Be sure to leave the pericranium down above the temporal line and the deep temporal fascia down over the temporalis muscle.
- Take care during the elevation that the vascular base of the flap is protected. All dissection in this area should be done with the artery and vein under direct vision.
- Mobilize the flap to the defect.
- This flap is easily skin grafted if required. Great care should be taken in placing tacking sutures from the skin graft to the flap to avoid injury to the vascular pedicle.
- Because the flap is thin, the zygomatic arch usually does not need to be divided to swing the flap into the desired position. Removal of the arch does add to the length and may decrease the potential for venous congestion.
- The scalp is closed over one or two suction drains with a subcutaneous stitch of 3-0 or 2-0 vicryl and skin staples. The scalp incision is dressed with antibiotic ointment, and no pressure dressing is applied. The preauricular skin incision is closed with 5-0 nylon.
Images


Postoperative Care
- Patient may carefully wash hair beginning around postoperative day 3 or 4. Mild baby shampoo is used, and antibiotic solution is reapplied to the incision line.
- Staples are removed at ten days.
- Glasses should not be worn or modified for several weeks. If they apply any pressure to the preauricular area, have the patient bring them in.
References
Abul-Hassan HS, Ascher GVD, Acland RD. Plast Reconstr Surg. 1986;77: 17-24.
Cheney ML, Varvares MA, Nadol JB. The temporoparietal fascial flap in head and neck reconstruction. Arch Otolaryngol Head Neck Surg. 1993;119: 618-623. (vm)
Cheney ML, Megerian CA, Brown MT, McKenna MJ. Mastoid obliteration and lining using the temporoparietal fascia flap. Laryngoscope 1995 Sep;105:1010-3.
David SK, Cheney ML. An anatomic study of the temporoparietal fascia flap. Arch Otolaryngol Head and Neck Surgery 1995 Oct;121(10):1153-6.