See also:
Protocol created June 12th, 2021 by Kothari DS, Hoffman HT, and Van Daele DJ
Definitions and Etiology
Vocal Fold Hemorrhage (VFH) results from the rupture of a submucosal blood vessel of the vocal fold usually associated with internal or external laryngeal trauma and may be associated with impaired coagulation (Lennon, 2013). The extravasated blood diffuses through the superficial layer of the lamina propria and either may remain asymptomatic or cause dysphonia due to the changes in the mass and rheologic properties of this layer (Kerwin, 2016). Both hemorrhagic polyps and non-hemorrhagic polyps have been reported to result from vocal fold hemorrhage with localized edema and organization into a polyp containing hyalinized stroma (Kotby 1988 and Altman 2007).
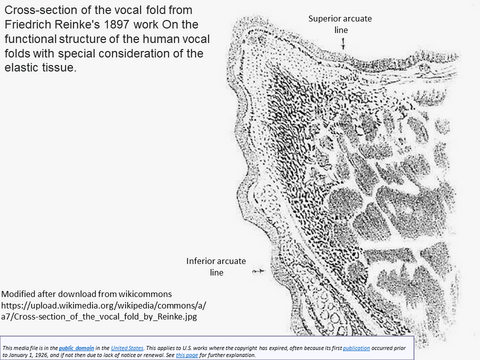
Histology of Reinke's Space
The vocal fold is composed of multiple layers: including the overlying fluid, the cover (epithelium, and lamina propria - divided into a superficial, intermediate and deep layers of the lamina propria) and the body (underlying musculature). The superficial lamina propria (SLP) is composed of loose fibrous components and extracellular matrices (Prades, 2009).
Reinke's space is the subepithelial compartment of the vocal fold evaluated by Friedrich Berthold Reinke in the 1890's through infusion of liquid into the space that now bears his name (Tavaluc 2019). The boundaries of Reinke's space - contained within the boundaries:
- Superficial: vocal fold epithelium
- Deep: vocal ligament
- Cranial: superior arcuate line
- Caudal: inferior arcuate line
- Anterior: Broyle's ligament
- Posterior: Arytenoid
Hirano (Hirano 1991, Sato 1999) pioneered the evaluation and naming of vocal fold structures in identifying the superfical layer of the lamina propria (synonymous with Reinke's space) as composed of amorphous substance that is loose and pliable underlying the epithelium and clearly delineated from the intermediate layer of the lamina propria which defines the medial border of the vocal ligament. The vocal ligament - comprised of the intermediate and deep layers of the lamina propria - has a gradual transition from dominance of elastic fibers in the intermediate portion to the more dense collagenous fibers that insert into the underlying vocalis muscle (thyroarytenoid) without clear demarcation.
Reinke's space is a potential space for accumulation of material as may occur with vocal fold hemorrhage (VFH). The SLP (aka Reinke's space) vibrates during phonation -- facilitated by the viscoelasticity of its extracellular matrix composed of reticular, collagenous and elastic fibers. VFH (vocal cord hemorrhage) disrupts this medium often resulting in impaired vibration.
The normal microcirculation to the vocal folds is dominated by capillaries in the superficial lamina propria with deeper layers containing arterioles and venules (Arens 2015).
The arcuate line (depicted in Reinke's coronal image of the vocal cord) is considered the border between squmous epithelium of the vocal fold and high columnar epithelium on the dorsal and ventral sides (Kutta 2006)

Presenting symptoms
The most common presenting symptom of VFH is sudden change in voice quality (Spiegel, 1996) with many cases of vocal fold hemorrhage asymptomatic and discovered incidentally in the course of examining the larynx. Dysphonia associated with vocal fold hemorrhage has been attributed to blood dissecting through the submucosal plane and to alter the vibration of the vocal fold. Spiegel et al identified the progressive development of hoarseness, voice fatigue and minor vocal changes, such as loss of range in upper register noticed while singing, as additional symptoms. Although symptoms from vocal fold hemorrhage by develop with sudden onset, slowly progressive dysphonia or vocal changes may also be a presentation due to slow leakage of blood from a vessel or after contralateral contact swelling of the vocal fold. Trauma to the peri-orbital region with blood extravasation results in discoloration that is often initially red then blue-violet "black-eye" with the color fading over days to yellowish-green before disappearing usualy over 1 to 2 weeks. A similar progression of discoloration may occur during resolution of a vocal fold hemorrhage.
Risk Factors
Risk factors for VFH include phono-trauma - such as vocalists may experience during a musical performance - or through other strenuous vocal fold activity as occurs with sustained loud talking (teachers, public speakers) or cheering at a sporting event (Paknezhad, 2019). Although many publications addressing VFH have focussed on vocalists, it is unclear whether the incidence is truly higher in such patients or if awareness of their voice change drives them to seek prompt evaluation. Among the general population, Kerwin et. al. propose that many VFH events resolve before they come to medical attention.
Those with vocal cord polyps, inflammatory changes of vocal cords, such as reflux laryngitis, and vocal cord varix can weaken areas within blood vessel walls and increase susceptibility (Paknezhad, 2019). Premenstrual hormonal status has been reported as a risk factor, possibly related to the presence of sex hormone receptors on the vocal folds and cyclical variations in laryngeal architecture related to hormone levels (Raj, 2010; Spiegel, 1996). Oral endotracheal intubation is another risk factor due to the anatomic passage of the tube through the vocal folds. Use of anticoagulation therapy - such as aspirin, clopidogrel, warfarin and apixaban - increases the risk of vocal fold hemorrhage.
Diagnosis
VFH is diagnosed by imaging the larynx through indirect mirror exam, flexible fiberoptic laryngoscopy, rigid transoral stroboscopy or microdirect laryngoscopy - usually performed in response to vocal complaints. VFH can also be found incidentally on routine surveillance, as depicted in the case below identifying followup after radiation for laryngeal cancer. Imaging of the vocal folds demonstrate discoloration that evolves over time often assocaited impaired mucosal wave during phonation with stroboscopy may specifically show a decrease in the amplitude or wave form (Spiegel, 1996).
Management and Risk of Recurrence
Standard treatment for VFH is avoidance of risk factors such as anticoagulation (discontinuing if possible), treatment of inciting factors (such as cough) and diminishing further phonotrauma as much as possible (voice rest/voice therapy). The duration and intensity of the recommended voice rest may be facilitated by a program of voice therapy - and depends on many factors that reflect the vocal demands and expectations that may determine management more than the physical findings. Oral steroids have been promoted by some as possibly useful to treat an acute hemorrhage - but without clear evidence supporting their use.
A repeat examination of the larynx (often flexible fiberoptic laryngoscopy) 7-10 days after the initial exam is a reasonable method or re-assessment for professional singers, but more intrusive than may be needed for those affected who are outside the category of professional voice.
Voice rest theoretically decreases the risk of permanent sequelae from vocal fold hemorrhage by limiting further dissection of blood in the submucosal plane and minimizing vocal fold trauma that may provoke a fibroblast mediated scar formation (Spiegel, 1996). The effectiveness of voice rest remains questioned (Kaneko 2017) - but may be facilitated by voice conservation with increased use of alternate communication methods such as writing, texting and email can be used. Cough suppressants, adequate hydration and minimal throat clearing are thought to additionally limit irritation of the vocal folds and augment the benefit voice rest for wound healing, though these have not been evaluated in clinical trial (Paknezhad, 2019).
Recurrent VFH can have a variety of underlying etiologies. In a retrospective cohort study of 47 patients with VFH, recurrence occurred in 26% of patients. Varix was identified with significant association with recurrence, at 48%, though this study's power is limited by sample size (Lennon, 2013). Another retrospective cohort study of 513 vocal performers presenting for vocal care were evaluated for the incidence of VFH and presence of varix or not (Tang, 2015). Varix was associated with a 10 fold increased risk of VFH at 12 months (cases of VFH per 1000 person-months) in comparison to non-varix patients. It is worth noting the incidence is low as only 2.68% of those with varix vs 0.8% of those without varix had VFH, and that a study involving a vocal performer cohort may not have great external validity.
A case report of vocal fold telangiectasia in a patient with dysphonia and history of hereditary hemorrhagic telangiectasia (HHT) offered the suggestion that prophylactic photoangiolytic laser therapy may diminish the risk of recurrence (Chang, 2014). Telangiectasia's are commonly seen after irradiation to the larynx as in the case presented below (Wang CC1978).
Other reported causes of recurrent vocal fold hemorrhage include harmful voice behaviors, such as excessively loud talking, tightening throat while talking and abusive singing patterns, and can be addressed with voice therapy and singing lessons (Spiegel, 1996). In cases of recurrence with known irregular blood vessels, such as varix, or vocal fold irregularities, microlaryngoscopy with KTP angiolytic laser or electrocautery treatment may be needed to coagulate abnormal blood vessels treat existing abnormalities and decrease future risk of to hemorrhage (see Hemorrhagic vocal cord polyp KTP laser treatment in clinic and Negative Pressure Face Shield (NPFS) for Transnasal Laryngoscopy KTP Laser Treatment of Hemorrhagic Polyp in COVID Era).
Woo (Woo 2018) was first to report vocal cord injection with hyaluronidase (Vitrase (Alliance Medical Products Inc., Irvine, CA) at 200 units/1 mL to treat three cases of acute vocal hemorrhage with early fusiform polyp formation as an in-office procedure employing videostroboscopic in two patients and under general anesthesia in one. Woo offered a rationale for use of hyaluronidase in the larynx as similar to that reported in the facial plastic and ophthalmology literature (Dunn 2010 and Cavallini 2013) - and identified its value in improving vascular permeability to absorb extravasation of hemorrhage and blood products as a process useful for selected patients employing a small needle injection into the superficial layer of the lamina propria (SLP). He identified a role for the hyaluronidase additionally in the treatment of over-injection of the vocal fold with hyaluronic acid and also patients with polypoid corditis.
Long-Term Implications
Isolated VFH often resolves without surgical intervention or long term consequences (Kerwin, 2016). A retrospective cohort study of 41 patients with VFH were administered Voice Handicap Index-10 (VHI-10) and Singing Voice Handicap Index (SVHI-10) surveys. After a median of 41 months follow-up, patients with VFH had favorable vocal function assessment and had no significant difference in VHI-10 and SVHI-10 scores when compared with controls without VFH. This study suggests VFH has no significant long-term impact on subjective voice quality or perception of vocal function. Kerwin et. al. acknowledge this study is limited by insufficient power and selection bias, as questionnaire post-VFH surveys were administered via telephone and may disproportionately select for patients with a favorable outcome after VFH.
Though most VFH results in temporary dysphonia as Kerwin et. al. state, many authors claim experience of permanent dysphonia, hoarseness and loss of vocal range secondary to submucosal scarring (Spiegel, 1996; Paknezhad, 2019). However, there are no documented cases of permanent dysphonia or video evidence of submucosal scarring in the professional literature (Kerwin, 2016).
Case Images
Incidental finding of VFH on follow-up 6 years after irradiation for T1 right vocal cord squamous cell carcinoma with recent anticoagulation initiated with Plavix
References
Lennon CJ, Murry T, Sulica L. Vocal fold hemorrhage: factors predicting recurrence. Laryngoscope. 2014 Jan;124(1):227-32. doi: 10.1002/lary.24242. Epub 2013 Jul 19. PMID: 23754508.
Spiegel JR, Sataloff RT, Hawkshaw M, Rosen DC. Vocal fold hemorrhage. Ear Nose Throat J. 1996 Dec;75(12):784-9. PMID: 8991228.
Paknezhad H, Ramadan O, Sataloff RT. Vocal Fold Hemorrhage. Ear Nose Throat J. 2019 Sep 30:145561319869914. doi: 10.1177/0145561319869914. Epub ahead of print. PMID: 31569976.
Tang CG, Askin G, Christos PJ, Sulica L. Vocal fold varices and risk of hemorrhage. Laryngoscope. 2016 May;126(5):1163-8. doi: 10.1002/lary.25727. Epub 2015 Oct 20. PMID: 26485065.
Kerwin LJ, Estes C, Oromendia C, Christos P, Sulica L. Long-term consequences of vocal fold hemorrhage. Laryngoscope. 2017 Apr;127(4):900-906. doi: 10.1002/lary.26302. Epub 2016 Oct 7. PMID: 27714858.
Raj A, Gupta B, Chowdhury A, Chadha S. A study of voice changes in various phases of menstrual cycle and in postmenopausal women. J Voice. 2010 May;24(3):363-8. doi: 10.1016/j.jvoice.2008.10.005. Epub 2009 Jan 29. PMID: 19185458.
Prades JM, Dumollard JM, Duband S, Timoshenko A, Richard C, Dubois MD, Martin C, Peoc'h M. Lamina propria of the human vocal fold: histomorphometric study of collagen fibers. Surg Radiol Anat. 2010 Apr;32(4):377-82. doi: 10.1007/s00276-009-0577-9. Epub 2009 Oct 20. PMID: 19841851.
Chang J, Yung KC. Dysphonia and vocal fold telangiectasia in hereditary hemorrhagic telangiectasia. Ann Otol Rhinol Laryngol. 2014 Nov;123(11):769-70. doi: 10.1177/0003489414538400. Epub 2014 Jun 9. PMID: 24913291.
Lin YH, Wang CT, Lin FC, Liao LJ, Lo WC, Cheng PW. Treatment Outcomes and Adverse Events Following In-Office Angiolytic Laser With or Without Concurrent Polypectomy for Vocal Fold Polyps. JAMA Otolaryngol Head Neck Surg. 2018 Mar 1;144(3):222-230. doi:
Woo P. Hyaluronidase Injection in the Vocal Folds for Vocal Hemorrhage, Reinke Edema, and Hyaluronic Acid Overinjection: A Novel Application in the Larynx. J Voice. 2018 Jul;32(4):492-498. doi: 10.1016/j.jvoice.2017.07.004. Epub 2017 Sep 1. PMID: 28867161.
Dunn A.L., Heavner J.E., Racz G. , et al. Hyaluronidase: a review of approved formulations, indications and off-label use in chronic pain management Expert Opin Biol Ther, 10 (2010), pp. 127-131
Cavallini M., Gazzola R., Metalla M. , et al. The role of hyaluronidase in the treatment of complications from hyaluronic acid dermal fillers Aesthet Surg J, 33 (2013), pp. 1167-1174
Golub JS, Hapner E, Johns MM 3rd. Vocal fold hemorrhage observed during laryngoscopy. Ear Nose Throat J. 2006 Mar;85(3):148. PMID: 16615590.
Kaneko M, Shiromoto O, Fujiu-Kurachi M, Kishimoto Y, Tateya I, Hirano S. Optimal Duration for Voice Rest After Vocal Fold Surgery: Randomized Controlled Clinical Study. J Voice. 2017 Jan;31(1):97-103. doi: 10.1016/j.jvoice.2016.02.009. Epub 2016 Aug 1. PMID: 27492336.
Christoph Arens, Cesare Piazza, Mario Andrea, Frederik G. Dikkers, Robin E. A. Tjon Pian Gi, Susanne Voigt-Zimmermann, Giorgio Peretti, Proposal for a descriptive guideline of vascular changes in lesions of the vocal folds by the committee on endoscopic laryngeal imaging of the European Laryngological Society, European Archives of Oto-Rhino-Laryngology, 10.1007/s00405-015-3851-y, 273, 5, (1207-1214), (2015).
Tavaluc R, Tan-Geller M. Reinke's Edema. Otolaryngol Clin North Am. 2019 Aug;52(4):627-635. doi: 10.1016/j.otc.2019.03.006. Epub 2019 May 14. PMID: 31101355.
Hirano M Chapter 4 "Phonosurgical Anatomy of the Larynx" pp 25-42 in PHONOSURGERY: Assessment and Surgical Management of Voice Disorders editors Ford CN and Bless DM Raven Press Ltd., New York, New York 1991
Sato K, Hirano M, Nakashima T. Electron microscopic and immunohistochemical investigation of Reinke's edema. Ann Otol Rhinol Laryngol. 1999 Nov;108(11 Pt 1):1068-72. doi: 10.1177/000348949910801108. PMID: 10579234.
Jovanovic MB, Milutinovic Z, Perovic J, Grubor A, Milenkovic S, Malobabic S. Vocal fold mucosa "blue lines" observed on contact telescopy at Reinke's edema. J Voice. 2009 Jul;23(4):512-5. doi: 10.1016/j.jvoice.2007.10.019. Epub 2008 Mar 17. PMID: 18346872.
Kotby M.N., Nassar A.M., Seif E.I., et. al.: Ultrastructural features of vocal fold nodules and polyps. Acta Otolaryngol (Stockh) 1988; 105: pp. 477-482.
Altman KW. Vocal fold masses. Otolaryngol Clin North Am. 2007 Oct;40(5):1091-108, viii. doi: 10.1016/j.otc.2007.05.011. PMID: 17765697
Kutta H, Steven P, Paulsen F. Anatomical definition of the subglottic region. Cells Tissues Organs. 2006;184(3-4):205-14. doi: 10.1159/000099628. PMID: 17409747.
Wang CC. Treatment of squamous cell carcinoma of the larynx by radiation. Radiol Clin North Am. 1978 Aug;16(2):209-18. PMID: 704815.
