Lung Imaging at Iowa Research Symposium
| Tentative Agenda | |
|---|---|
| 8 a.m. | Coffee and light snacks |
| 8:45 a.m. | Introduction and welcome |
| 9 a.m. | Dr. Benjamin Smith, McGill University and Columbia University |
| 10 a.m. | Dr. Jacob Herrman, The University of Iowa |
| 10:30 a.m. |
Lightning talks from T32 trainees Adam Galloy, Carley Stewart, Emmanuel Akor, Kevin Knoernschild |
| 11 a.m. | Dr. Jason Woods, Cincinnati Children's Hospital |
| Noon | Lunch |
| 1 p.m. | Introduction to afternoon session |
| 1:15 p.m. | Dr. Marrissa McIntosh, Western Ontario University |
| 1:45 p.m. |
Lightning talks from T32 trainees Wahidul Alam, Riley Meyer, Zachary Althof, Erik Cole, Qi Wang |
| 2:15 p.m. | Poster session with coffee and snacks |
| 3:15 p.m. | Closing |
Speakers

Ben Smith is a pulmonary physician and scientist with appointments at Columbia University and McGill University in Montreal, Canada. His training includes pulmonary medicine, physiology and epidemiology. His research program applies quantitative lung imaging to understand why some people develop lung disease and other people do not. His recent work investigates the remarkable variation in native lung structure and its relationship to disease susceptibility across the lifespan.

Jacob Herrmann joined the Roy J. Carver Department of Biomedical Engineering in the Fall of 2022. Dr. Herrmann received BS and MS degrees in Biomedical Engineering from Boston University, and the PhD in Biomedical Engineering from the University of Iowa. Dr. Herrmann conducted postdoctoral fellowships at Boston University and at University of Iowa (as part of the T32 Lung Imaging Training Program). Dr. Herrmann also co-founded OscillaVent, Inc., to translate his graduate thesis work into a commercializable medical device for mechanical ventilation.
Dr. Herrmann’s research interests encompass measurement, modeling, and control of dynamical systems involving multiscale phenomena and emergent behavior from complex interactions. Our lab’s current research objectives focus on elucidating the biomechanical conditions that drive lung injury and disease progression, and evaluating new therapeutic strategies to improve patient care. We use dynamic image reconstruction techniques to quantify the structural deformations of lung tissues during precision-timed mechanical ventilation or breathing-like stretch, capturing multiscale respiratory dynamics ranging from organ-level mechanics down to the interactions between individual collagen and elastin fibers.

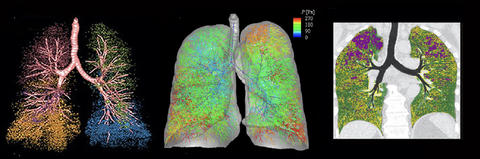
My interest in pulmonary imaging research was born of a unique background in hyperpolarized gases and atomic physics, combined with an interest in translational applications to surgery and pulmonary medicine.
My primary research areas include pulmonary MRI, regional structure-function relationships, pathophysiology, translational imaging research and clinical trials. The overall goal of this research is to improve outcomes for patients with lung disease through precise imaging and determination of regional structure-function relationships, using a combination of translational techniques and innovative methodologies.
We have pioneered 129Xe MRI in pediatrics and help lead the 129Xe MRI Clinical Trials Consortium. We also have begun to redefine bronchopulmonary dysplasia (BPD) by imaging-phenotypes, which show a direct relationship to outcomes.
Our research team is comprised of experts in hyperpolarized-gas MRI and in the use of this technique to measure regional lung function, physiology and microstructure. Many of the fellows and junior faculty that I have mentored have won awards and recognition from national and international organizations, such as the International Society for Magnetic Resonance in Medicine (ISMRM), the American Thoracic Society (ATS) and the Society for Pediatric Radiology (SPR).
Since my arrival at Cincinnati Children’s in 2013, I’ve served as the director of the Center for Pulmonary Imaging Research (CPIR). Our center offers a multidisciplinary research and training program that combines pulmonary medicine, radiology and neonatology. I also co-lead the Bronchopulmonary Dysplasia Center at Cincinnati Children’s, where imaging research has been rapidly translated into clinical care and improved patient outcomes.

Dr. Marrissa McIntosh previously completed her PhD in Medical Biophysics at Western University under the supervision of Dr. Grace Parraga. Her primary research focus is to evaluate eosinophilic asthma patients and their response to biologic therapy using advanced imaging technologies including 129Xe MRI and chest CT.
| Poster Session | |
|---|---|
| Kimberly Schroeder | Don't Judge a Nodule by Its Looks: Evaluation of Lung Cancer Risk Prediction Models |
| Daniel Meggo | Quantifying temporal dynamics of alveolar recruitment during mechanical ventilation |
| Faizyab Chaudhary | Single Volume Surrogates of Lung Function through Generative Adversarial Learning |
| Carley Stewart | Spatial Analysis of Mucociliary Transport Patterns |
| Kevin Knoernschild | Development of a Radiomics Machine Learning Model for Lung Cancer Screening Utilizing Low Dose CT |
| Qi Wang | In Vitro 2.5D System for Studying Mechano-chemical processes that drive lung remodeling and fibrosis |
| Adam Galloy | Characterization of lung lobar sliding kinematics using finite element modelling and helmholtz-hodge decomposition |
| Jian Gao | Assessing the Mechanical Properties of Acutely Injured Lungs: A Comparative Study of Traditional and Novel Ventilation Techniques |
| Emmanuel Akor | Utilizing Computed Tomographic (CT) Imaging Mechanical Characteristics of the Acutely Injured Lung: A Quantitative CT Imaging Assessment |
| Hira Awan | QCT texture biomarkers are associated with all cause mortality in SPIROMICS and COPDGene |
| Erik Cole | Graph Neural Networks for Correlating Airway Structural Features with COPD Severity |
| Jake Kitzmann | Semi-Automated Segmentation of Pulmonary Nodules |
| Keegan Staab | Regional Correlation of Pulmonary Gas Exchange and Perfusion in IPF using MRI |
| Soheil Hosseini | AI-Assisted CT-based Characterization of Pulmonary Arterial and Venous Trees |
| Wahidul Alam | Accelerated Imaging of Airway Collapse in Obstructive Sleep Apnea: Utilizing Generative variational Manifold Learning in Synergy with a Custom Upper Airway Coil and Variable Density Spirals |
| Natally AlArab | Optimizing Chest CT with Photon-Counting Detector Technology: Comparison to Established Energy-Integrating Detector CT Protocols |
| Suchet Anand | Relationships between Lung Inflammation, Measures of Cognition, and Brain MRI in Heavy Smokers |
| Jonathan Percy | Assessment of Ventilation and Gas Exchange in Long COVID Using Hyperpolarized Xe and Quantitative CT |
| Zachary Altof | Anomaly Detection for Fissure Integrity Analysis Screening |
| Xuan Zhang | Identification of Sub-clusters of Post-COVID-19 Subjects using a Contrastive Deep Learning Approach |
Individuals with disabilities are encouraged to attend all University of Iowa–sponsored events. If you are a person with a disability who requires a reasonable accommodation in order to participate in this program, please contact Kim Glynn in advance at (319)384-1024 or kimberly-a-glynn@uiowa.edu